Healthy Mothers and Healthy Newborns: The Vital Link
(April 2002) The past century witnessed a revolution in health care, yet millions of women still endure the risks of pregnancy and childbirth under conditions virtually unchanged over time. Maternal complications take a serious toll on women. Tragically, millions of stillbirths and newborn deaths result from many of the same preventable causes.
Every year, 4 million babies are stillborn. Another 4 million newborns die before they reach the first month of life.1 As with maternal deaths, 98 percent of newborn deaths occur in developing countries. While there have been significant declines in infant and child mortality in the developing world in recent decades, there has been little progress in reducing the death rate for mothers and newborns. As a result, newborn deaths now represent 40 percent of all deaths among children under 5 years of age.2 To sustain previous health gains and meet the United Nations Millennium Development Goals, policymakers need to place much greater emphasis on proven, cost-effective measures to save maternal and newborn lives.
Making motherhood safer is critical to saving newborns. Research shows that a significant number of stillbirths and neonatal deaths could be prevented if all women were adequately nourished and received good quality care during pregnancy, delivery, and the postpartum period.3 But safe motherhood is only one part of the equation. Policymakers must ensure that health care is available for newborns as well as their mothers. From the moment of birth, each newborn is a separate individual with needs that may depend not only on the mother, but also may require special attention.
Newborn Health Begins With Mothers
To a considerable extent, the well-being of a newborn depends on the health of the mother. In developing countries, a mother’s death in childbirth means almost certain death for her newly born child. When mothers are malnourished, sickly, or receive inadequate prenatal and delivery care, their babies face a higher risk of disease and premature death. The rate of neonatal death is thus high in regions where the risk of maternal death is high (see Table 1). Recent estimates show that in Africa, for example, a woman’s risk of dying from maternal causes over her lifetime is one in 19; and one of every five African women risks losing a newborn during her lifetime.4 Neonatal and maternal deaths place a significant burden on health systems as well as on women and families. A recent report revealed the extent of loss of healthy life from newborn deaths; for example, it represents more than 8 percent of the total disease burden in sub-Saharan Africa and nearly 14 percent in South Asia.5
Table 1
Lifetime Risks to Mothers
| Lifetime risk that a woman will lose a newborn* | Lifetime risk that a woman will die of maternal causes | |
|---|---|---|
| Africa | 1 in 5 | 1 in 19 |
| Asia | 1 in 11 | 1 in 132 |
| Latin America | 1 in 21 | 1 in 188 |
| More developed countries | 1 in 125 | 1 in 2,976 |
* Deaths to babies between birth and 28 days.
Source: Calculated from most recent rates available from Save the Children (neonatal mortality), Population Reference Bureau (total fertility rate), and UNICEF (maternal mortality ratio).
The survival and well-being of newborns depend on their mothers in several critical ways.
Birth Spacing and Newborn Survival
First, newborn health is affected by the timing and frequency of pregnancy. Women who give birth when they are too young or too old, or have babies too closely spaced, place themselves and their newborns at increased risk of complications. Research clearly highlights the association between newborn and infant mortality and birth interval. Infants born less than two to three years apart are significantly more likely to die. For example, a newborn who is less than 24 months younger than the next oldest sibling is 2.2 times more likely to die than a newborn who arrives after 36 months (see Figure 1).6 In addition, women who have borne many children are at a higher risk of maternal mortality, and their newborns are at increased risk of death as well. Effective use of family planning methods can contribute to improved maternal and newborn health by helping women avoid pregnancy when the risk of a poor outcome is high.
Figure 1
Newborn Deaths and Short Birth Intervals
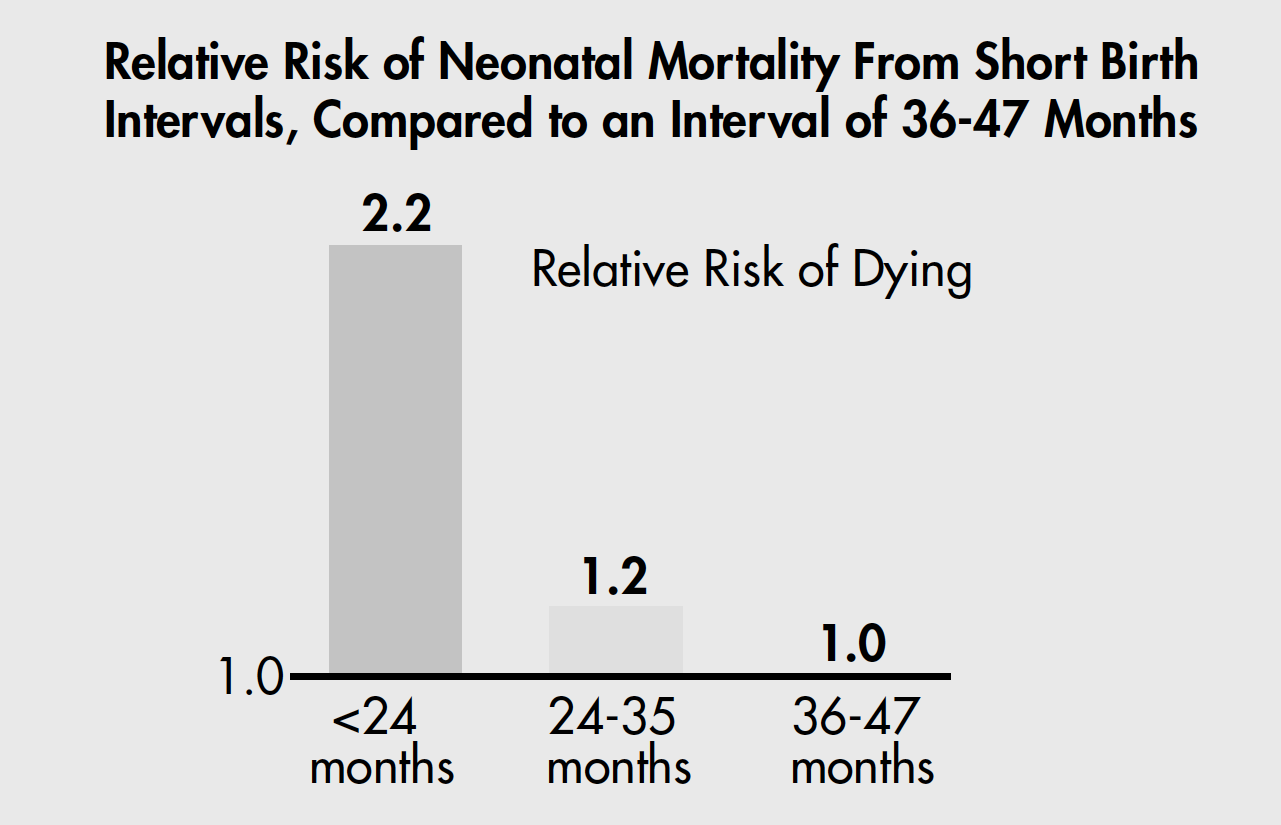
Source: Data from Demographic and Health Surveys from 17 countries, calculated by Shea Rutstein, MACRO International, Inc.
Complications of Childbirth
Second, complications of childbirth can have a significant impact on newborns. Almost 30 percent of neonatal deaths are the result of injuries sustained during delivery.7 Asphyxia, for example, occurs when the newborn receives an inadequate supply of oxygen immediately before, during, or just after delivery. It is often caused by obstructed labor, a complication that also causes about 8 percent of maternal deaths. An estimated 4 million to 5 million newborns suffer from birth asphyxia and more than 1 million die from it. More than a million of those who live suffer consequences such as epilepsy, cerebral palsy, and developmental delay. Obstructed labor and asphyxia may go unrecognized and untreated because only about half of deliveries in less developed countries take place with the assistance of skilled health personnel who can detect, treat, or ensure referral care for the life-threatening complications of pregnancy and childbirth and the postnatal period (see Figure 2).8
Figure 2
Newborn Deaths and Skilled Care at Delivery
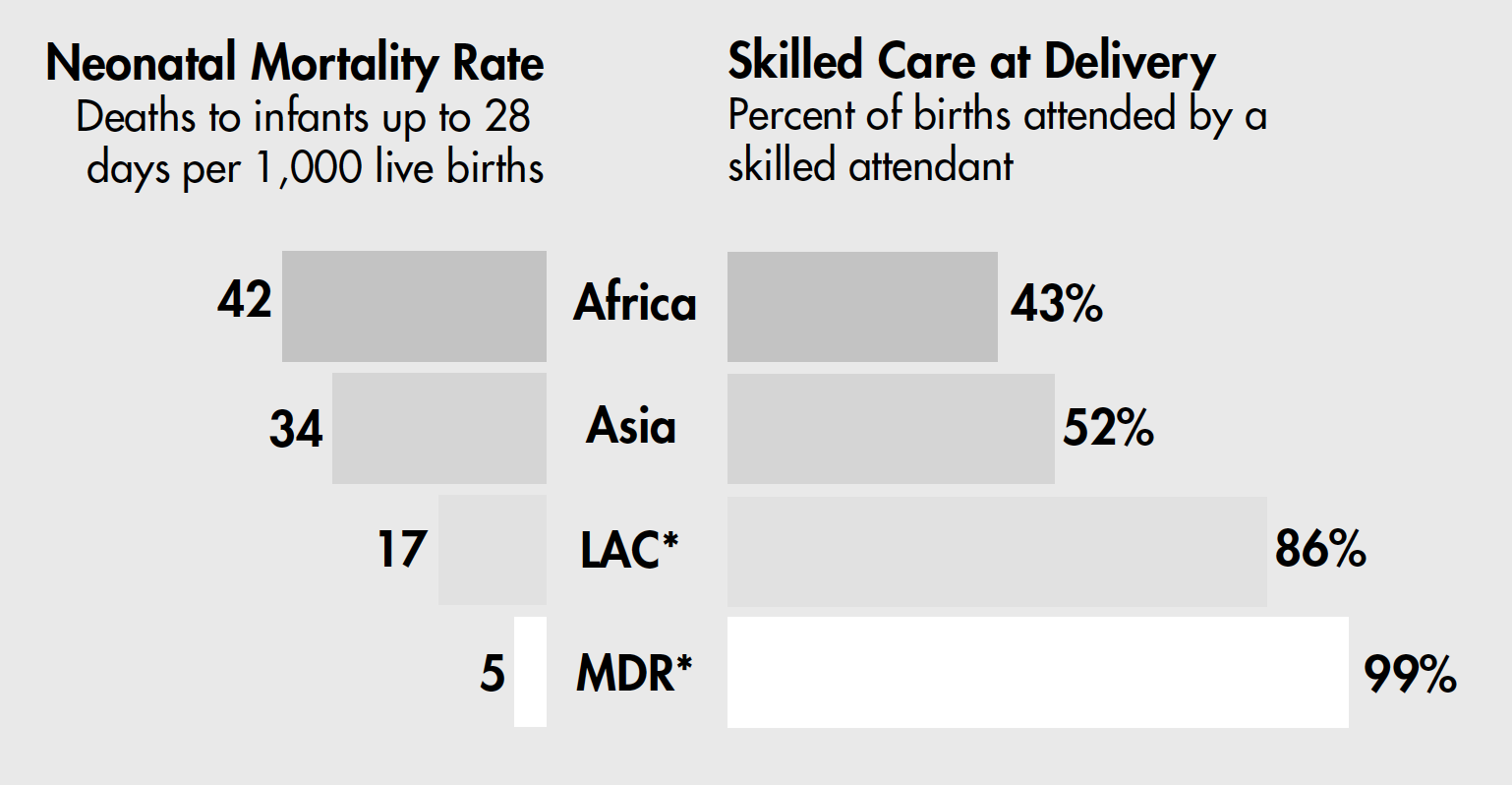 LAC*: Latin America and the Caribbean; MDR*: More developed regions.
LAC*: Latin America and the Caribbean; MDR*: More developed regions.
Source: Save the Children and Population Reference Bureau calculations.
Impact of Maternal Infections
Third, many stillbirths and newborn deaths from infection can be prevented through appropriate maternal care. Mothers may pass sexually transmitted infections to their newborns during pregnancy, delivery, or breastfeeding. Up to one-third of untreated HIV-positive mothers transmit the virus to their infants during the perinatal period (between 22 weeks of pregnancy and the first week of life), resulting in nearly a half-million child deaths in 1999.9 Some sexually transmitted infections can lead to blindness, and others are associated with stillbirth, low birth weight, and a variety of other complications after birth.
In countries where malaria is endemic, women are more likely to have it during pregnancy than at any other time. Infected women are more likely to have low birth-weight infants, a major risk factor for neonatal death. Malaria can cause up to 30 percent of preventable low birth weight and as much as 5 percent of neonatal mortality. Malaria is also associated with spontaneous abortion and stillbirth, and women who develop severe anemia from malaria are at increased risk of maternal death.10 In addition, pregnant mothers who have malaria and are HIV-positive are more likely to pass on their HIV status to their unborn child.11
Tetanus is another illness that affects both mothers and newborns. Infants are at increased risk of contracting the disease when their umbilical cords are cut with unclean instruments or treated with unhygienic traditional applications such as cow dung. Neonatal tetanus kills about 215,000 infants each year.12 Mothers are also susceptible to tetanus if their deliveries are unhygienic.
The Nutrition Link
Fourth, the nutritional status of girls and women, even long before pregnancy, affects fetal development and newborn health. Almost one-quarter of newborns in the developing world start life with some degree of impaired growth and micronutrient status.13 This condition is largely determined by the nutritional status of the mother. Impaired growth in the womb predisposes infants to have low birth weight, a condition affecting more than 20 million infants in the developing world every year.14 Low birth-weight infants who survive may suffer cognitive impairment, developmental problems such as poor attention span, and a much higher burden of disease and early mortality as adults than their counterparts who are born with normal weight.
Malnutrition often follows an intergenerational cycle, and many women enter pregnancy malnourished (see Figure 3). During pregnancy, they may not gain enough weight, which puts their babies at risk for low birth weight. Baby girls born underweight often grow up to be short, underweight adults. Very short women are more likely to have obstructed labor, which is dangerous for both their own health and that of their newborns. And thus the cycle continues.
Figure 3
Poor Nutrition Throughout the Life Cycle
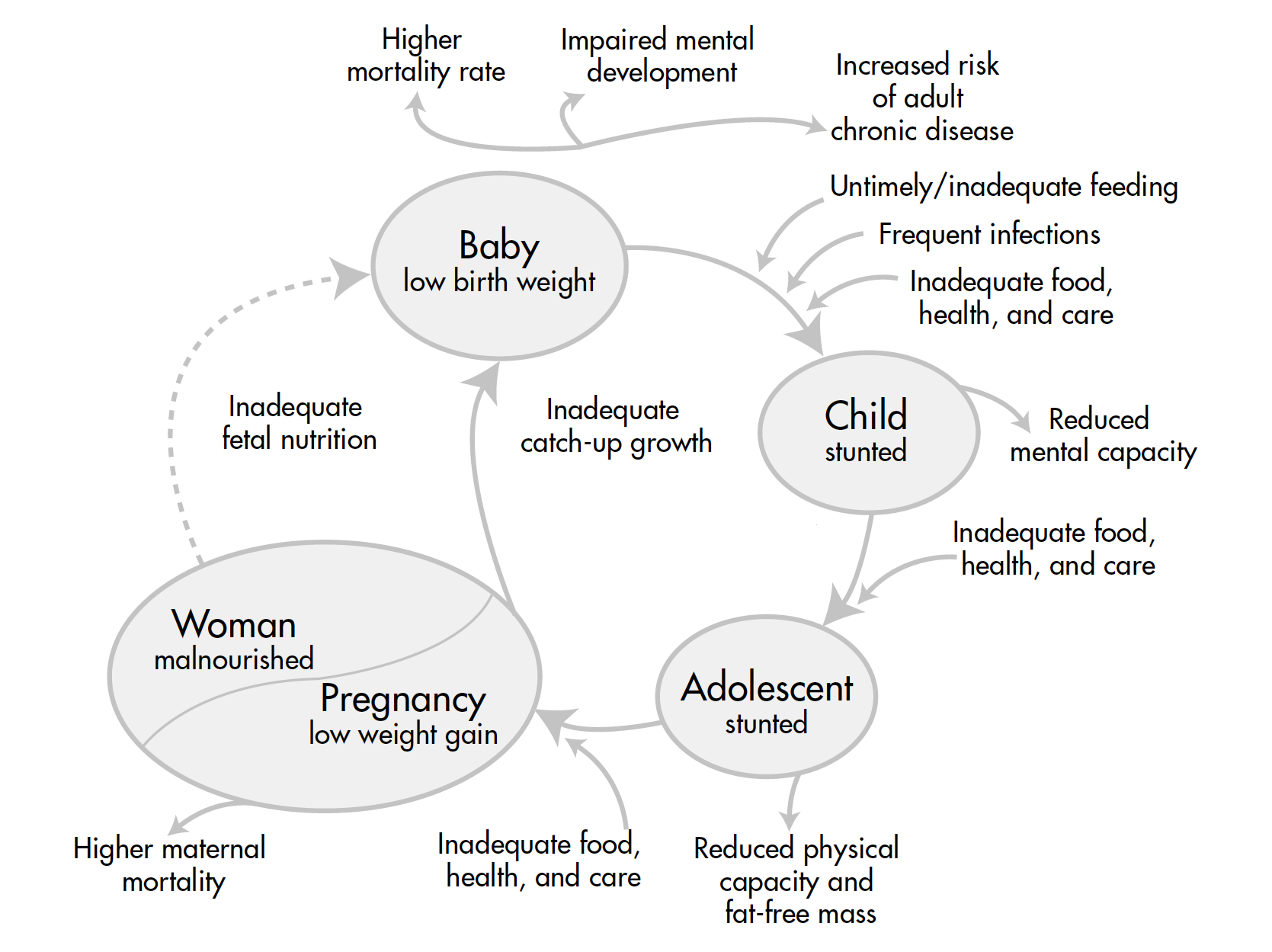 Source: Adapted from the ACC/SCN-appointed Commission on the Nutrition Challenges of the 21st Century.
Source: Adapted from the ACC/SCN-appointed Commission on the Nutrition Challenges of the 21st Century.
Micronutrient deficiencies also influence both maternal and neonatal health. For example, iron deficiency anemia afflicts about half of all pregnant women in developing countries.15 Mothers with severe anemia are at increased risk of maternal death, stillbirth, and early neonatal death; and their infants are at increased risk of low birth weight, prematurity, and/or cognitive impairments.
What Can Policymakers Do?
Research indicates that the cost-effective prenatal and delivery services that improve women’s health and nutrition could save a significant percentage of their newborns as well. However, it is important to recognize that during the postpartum period — when most deaths occur — mothers and newborns require individualized attention. Health care must be structured to meet the specific needs of the newborn as well as those of the mother.
Provide Skilled Care
Skilled attendance during labor and delivery can save newborn lives. For example, managing obstructed labor and severe antepartum bleeding can prevent asphyxia in newborns.16 Many of the newborns who have difficulty establishing breathing at birth can be rescued if attendants are trained in simple resuscitation methods. Providing a clean delivery, including clean cutting of the umbilical cord, is also essential for the health of mothers and neonates; it protects against sepsis in mothers and neonatal tetanus and sepsis in newborns. Immediate drying and warming of newborns through skin-to-skin contact is an effective way to prevent hypothermia and to promote immediate breastfeeding. Functioning referral care and transport systems must be available for managing maternal and newborn complications.
Promote Postnatal Care
The early postnatal period is a vulnerable time for both mothers and newborns. Sixty-one percent of maternal deaths occur during the first six weeks after birth, and nearly half of those deaths take place during the first day after delivery.17 Two-thirds of neonatal deaths occur in the first week of life, and two-thirds of those die within the first 24 hours.18 Immediate breastfeeding, which helps mothers by stimulating the contractions of the uterus that protect against severe bleeding, also protects infants by providing nutrients and essential immunities from disease. Exclusive breastfeeding, not supplemented with other foods or liquids, is particularly effective at preventing infection in newborns, yet rates are extremely low in developing countries.19 HIV-positive mothers need counseling on appropriate care and feeding of their newborns, as well as attention to the related infections they and their newborns may develop.
Some traditional practices, such as giving newborns cold baths and breast-milk substitutes soon after birth, are harmful. Education for families and communities about how to care for newborns and how to recognize health problems among mothers and newborns that require immediate attention is essential to improving maternal and newborn health.
Prevent and Treat Maternal Infections
Immunizing women of reproductive age with the tetanus toxoid vaccine protects both women and newborns. Tetanus toxoid is one of the safest, most effective, and least expensive vaccinations available. It can prevent tetanus infection in mothers during childbirth, and it passes immunity on to the fetus.
Preventing malaria also protects mothers and newborns. The World Health Organization recommends preventive treatment of pregnant women and making bed nets dipped in insecticide available to prevent transmission of malaria from mosquitoes in highly endemic areas. Treatment for infected mothers should also be included in antenatal care.
Testing and treatment for sexually transmitted infections should be part of antenatal care. Primary care facilities and family planning clinics can also work to prevent sexually transmitted infections through education, diagnosis, and treatment. Where HIV is prevalent, women should have access to voluntary counseling and testing. HIV-positive women should have access to short-course antiretroviral therapy and counseling on infant feeding options. Caregivers should provide HIV-negative mothers with counseling about safe practices to prevent contracting the infection. Becoming infected during pregnancy heightens the risk of transmitting the virus to newborns.
Break the Cycle of Poor Nutrition
The role of good nutrition in improved neonatal and maternal survival extends beyond the time a woman is pregnant. Promoting adequate nutrition and counseling women to gain enough weight during pregnancy is just the first step. Promoting a healthy and varied diet through an adequate supply of food will also improve the nutrition of girls and women over time. Some countries have addressed micronutrient malnutrition by fortifying foods (such as putting iodine in salt) or by providing iron and folic acid supplements, and — where appropriate — vitamin A, iodine, and zinc.
Integrate Interventions for Maternal and Newborn Survival Into Other Programs
Increasing access to contraceptives allows women to plan the number and timing of their pregnancies. Strengthening services to detect and treat sexually transmitted diseases, malaria, and malnutrition during pregnancy are also ways to protect both mothers and their newborns.
Gathering data on tetanus immunization rates, skilled attendance at delivery, low birth weight, breastfeeding practices, postpartum care, and other indicators of maternal and newborn health allows policymakers to make informed decisions about how to allocate funds.
Decisionmakers can improve maternal and neonatal health by supporting programs that emphasize education and fight against gender discrimination. Participating with communities, especially with women’s groups, to identify maternal and newborn health problems and then develop creative solutions together will also lead to improved maternal and neonatal health.22
Conclusion
Newborns are the most vulnerable members of society. Preventing newborn deaths and improving newborn health and survival go hand in hand with promoting safer motherhood. Decisionmakers can work to ensure healthier futures for mothers and their newborns by supporting programs that provide essential maternal and newborn care, as well as broader policies that enhance women’s health and socioeconomic opportunities during the life cycle. Intervening to make motherhood safer and to protect newborns in their most fragile period is an essential investment in the future.
References
- World Health Organization estimates, based on data collected around 1999.
- William Moss et al., “Research Priorities for the Reduction of Perinatal and Neonatal Morbidity and Mortality in Developing Country Communities,” Journal of Perinatology (forthcoming).
- Anne Tinker, “Safe Motherhood is a Vital Social and Economic Investment,” paper prepared for Technical Consultation on Safe Motherhood, Oct. 18-23, 1997.
- World Health Organization (WHO), United Nations Children’s Fund (UNICEF), and United Nations Population Fund (UNFPA), Maternal Mortality in 1995: Estimates Developed by WHO, UNICEF and UNFPA (Geneva: WHO, 2001).
- Adnan A. Hyder et al., “The Burden of Disease from Neonatal Mortality in Sub-Saharan Africa and South Asia,” report submitted to Save the Children.
- Shea Rutstein, “Effects of Birthspacing on Mortality and Health: Multivariate Cross-Country Analysis,” presentation by MACRO International, Inc., at the U.S. Agency for International Development, July 2000; and B.P. Zhu et al., “Effect of the Interval between Pregnancies on Perinatal Outcomes,” New England Journal of Medicine 340 (1999): 589-94.
- T. Kusiako, Carine Ronsmans, and L. Van der Paal, “Perinatal Mortality Attributable to Complications of Childbirth in Matlab, Bangladesh,” Bulletin of the World Health Organization 78 (2000): 621-27.
- Safe Motherhood Inter-Agency Group, Skilled Care During Childbirth: A Review of the Evidence (New York: Family Care International, forthcoming).
- Ellen G. Piwoz et al., Early Breastfeeding as an Option for Reducing Postnatal Transmission of HIV in Africa: Issues, Risks, and Challenges (Washington, DC: Academy for Educational Development, August 2001).
- David Rush, “Nutrition and Maternal Mortality in the Developing World,” American Journal of Clinical Nutrition 72 (Supplement, 2000): S212-40.
- Elizabeth A. Preble and Ellen G. Piwoz, “Prevention of Mother-to-Child Transmission of HIV in Africa: Practical Guidance for Programs” (Washington, DC: Academy for Educational Development, June 2001).
- UNICEF/WHO/UNFPA, “Maternal and Neonatal Tetanus Elimination by 2005: Strategies for Achieving and Maintaining Elimination,” accessed online at www.unfpa.org/tpd/publications/matetanuseng.pdf.
- Administrative Committee on Coordination (ACC)/Sub-Committee on Nutrition (SCN) and International Food Policy Research Institute, Fourth Report on the World Nutrition Situation (Geneva: UN/ACC/SCN, 2000).
- Saving Newborn Lives, State of the World’s Newborns (Washington, DC: Save the Children, 2001).
- Lindsay H. Allen, “Anemia and Iron Deficiency: Effects on Pregnancy Outcomes,” American Journal of Clinical Nutrition 71 (Supplement, 2000): S1280-84.
- Anne Tinker, “Healthy Mothers — Healthy Babies,” World Bank PHN Notes 2, no. 9 (Dec. 4, 1992).
- X.F. Li et al., “The Postpartum Period: The Key to Maternal Mortality,” International Journal of Gynecology & Obstetrics 54 (1996): 1-10.
- Joy Lawn, Brian J. McCarthy, and Susan Rae Ross, The Healthy Newborn: A Reference Manual for Program Managers (Atlanta: Centers for Disease Control, CARE, Care/CDC Health Initiative, 2001). More information can be found at www.cdc.gov/nccdphp/drh.
- Patricia Haggerty and Shea Rutstein, “Breastfeeding and Complementary Infant Feeding, and the Postpartum Effects of Breastfeeding,” DHS Comparative Studies no. 30 (Calverton, MD: MACRO International, Inc., 1999).
- UNICEF/WHO/UNFPA, “Maternal and Neonatal Tetanus Elimination by 2005.”
- Saving Newborn Lives, State of the World’s Newborns: Pakistan (Islamabad: Save the Children U.S.A., October 2001).
- Kathleen O’Rourke, Lisa Howard-Grabman, and Guillermo Seone, “Impact of Community Organization of Women on Perinatal Outcomes in Rural Bolivia,” Pan American Journal of Public Health (Revista Panamericana de Salud Pública) 3, no. 1 (1998): 9-14.
This brief is the first in the “Policy Perspectives on Newborn Health” series, produced through collaboration between the Population Reference Bureau and Save the Children’s Saving Newborn Lives initiative. Aimed at government decisionmakers and health care professionals, “Policy Perspectives on Newborn Health” will show how incorporating newborn care into existing safe motherhood and child survival programs can ensure newborn survival, as well as contribute to improving women’s health and the well-being of future generations. Saving Newborn Lives, launched with a generous contribution from the Bill & Melinda Gates Foundation, is a 15-year initiative to improve the health and survival of newborns in the developing world.
Anne Tinker of Save the Children and Elizabeth Ransom of the Population Reference Bureau (PRB) prepared this brief. Special thanks are due to the following reviewers: Robin Bell, Oona Campbell, Anthony Costello, Patricia Daly, Gary Darmstadt, Leslie Elder, Rae Galloway, Joy Lawn, Rebecca Lowery, Judith Moore, Vinod Paul, Suzanne Prysor-Jones, Catherine Shaw, Mary Ellen Stanton, Donald Wilson, and Nancy Yinger.
Box 1
Eliminating Neonatal Tetanus in Pakistan
Pakistan has recently launched a program to combat neonatal tetanus, which currently claims the lives of an estimated 21,000 Pakistani infants every year.20 Because the country has the world’s third-highest burden of death due to neonatal tetanus, this new project is underway to increase tetanus immunization coverage among women of childbearing age.21 Through the project, a collaborative effort among the Pakistan Ministry of Health, UNICEF, the Japan International Cooperation Agency (JICA), and Save the Children, about 4.5 million women in 57 districts are being vaccinated where neonatal tetanus is still a major public health problem. The project relies on local “lady health workers,” who go door-to-door giving tetanus toxoid vaccinations to all women of childbearing age. This strategy has succeeded in large part through a nationwide public information campaign targeting young women and critical decisionmakers at the national and community levels.
Box 2
Home-Based Newborn Health Care in India
In the Gadchiroli district of India, Drs. Abhay and Rani Bang and colleagues at the Society For Education, Action & Research in Community Health (SEARCH) have developed a remarkable approach to home-based health care that benefits both newborns and their mothers. It had to be home-based because 83 percent of births in rural India occur at home, and these villagers have virtually no access to health facilities. After two years of research, SEARCH introduced neonatal care through trained village health workers and trained birth attendants, who provide health education to new mothers, support breastfeeding and maintenance of body temperature, and recognize danger signs in mothers and babies. By the third year of the program, which tracked results in 39 intervention villages and 47 control villages, SEARCH had recorded a 62 percent reduction in the neonatal mortality rate for the intervention areas as well as a significant reduction in various neonatal and maternal morbidities. Saving Newborn Lives is currently testing the adaptability and sustainability of this approach, which SEARCH hopes will provide a creative initiative for similar organizations throughout the developing world.