Paola Scommegna
Contributing Senior Writer

April 23, 2018
Contributing Senior Writer
First in a series of three articles excerpted from “Health and Working Past Traditional Retirement Ages,” Today’s Research on Aging, Issue 37.
By 2030, when the last of the large baby boom generation (born 1946 to 1964) has reached their mid-60s, more than 21 percent of the U.S. population is projected to be age 65 or older—up from about 15 percent in 2016.
The greying of America increases the costs of public programs for older adults and shifts the balance between working people supporting those programs and retirees receiving benefits. The old-age support ratio—the number of working-age adults ages 18 to 64 for every adult age 65 or older—is on course to shrink dramatically from 4.1 in 2016 to 2.8 by 2030. To relieve this fiscal pressure, policymakers continue to discuss new financial incentives to encourage people to postpone retirement, such as further raising the eligibility age for Social Security (currently age 67 for those born after 1960) and Medicare (now age 65).
Working longer can reduce public spending and enable some older workers to enter retirement with more financial security. Estimates based on past health trends suggest that most U.S. older adults can work an extra two years before retiring.1But a growing body of research suggests that baby boomers in their 50s and 60s are in poorer health—with more chronic disease and disability—than earlier generations at the same ages, potentially affecting their capacity to work longer.
Older adults ages 51 to 61 had a higher prevalence of six out of eight chronic conditions—including 37 percent higher diabetes prevalence—in 2004-2010 than their peers in 1992-1998, a 2016 study finds.2 Hiram Beltrán-Sánchez of the University of California-Los Angeles, Marsha Jiménez of Brown University, and S.V. Subramanian of Harvard University analyzed self-reported chronic disease in the 1990s and 2000s using data from the nationally representative U.S. Health and Retirement Study (HRS). Based on their findings, they argue that older adults nearing traditional retirement ages appear more burdened by health conditions than several decades ago.
In another recent study, a University of Southern California research team finds Americans are living longer with more disability. Eileen Crimmins, Yuan Zhang, and Yasuhiko Saito examined life expectancy trends and disability rates in the 40-year period from 1970 to 2010.3They show that the average total lifespan increased for both men and women, but so did the proportion of time spent living with a disability. For people ages 65 and older, they identify a “compression of morbidity”—that is, a reduction in the proportion of life spent with disability. However, people in their prime working years (ages 20 to 64) experienced increases in the proportion of life spent with a disability. The researchers argue that there is “little evidence” of improvements in health “that would support increasing the age at retirement.”
In addition, a 2012 study that synthesized the results of five nationally representative surveys finds increasing disability among those ages 55 to 64 between 2000 and 2008 (a group that included the oldest baby boomers).4 During the same period, disability levels continued to decline among the oldest Americans (ages 85 and older) and held steady among those ages 65 to 84.
Linda Martin of the RAND Corporation, and Robert Schoeni of the University of Michigan also document rising disability levels between 1997 and 2010 among middle-age and older Americans (ages 40 to 64).5 Their analysis, based on the nationally representative National Health Interview Survey data, identifies a link between increasing obesity and rising disability.
Martin and Schoeni take this line of research further, teaming up with HwaJung Choi of the University of Michigan for a 2016 study focusing on 55-to-69-year-olds using HRS data for 1998 to 2010.6 They find no improvement in levels of physical functioning and activity limitations during the period, and some evidence of worsening. They show that obese individuals face a greater likelihood of having physical limitations. Although baby boomers are less likely to smoke, have emphysema, or have heart attacks, they are more likely to be obese or have diabetes or high blood pressure than the previous generation at similar ages, they report.
Obesity is a risk factor for a variety of chronic conditions; it may also increase the likelihood of early retirement due to disability. Using HRS data, Francesco Renna and Nidhi Thakur of the University of Akron find that men and women under age 65 who were obese in 1992 were more likely to have a disability and retire early by 2002.7
“Obesity can largely impact labor market decisions directly through impairment of bodily functions and indirectly by being a risk factor for various diseases like hypertension, arthritis, etc.,” they write. About two in five Americans (43 percent) in their 40s and 50s were obese in 2015-2016, and thus face an increased risk of retiring early because of a disability or poor health.8
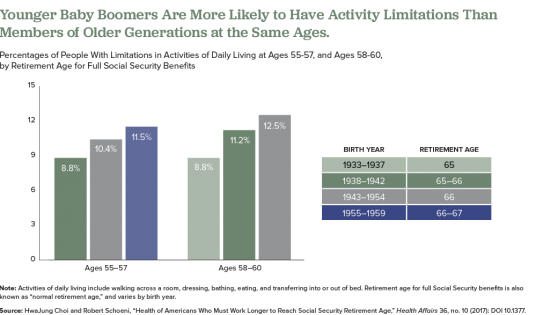
In a 2017 study, Choi and Schoeni examined trends in both physical limitations and cognitive impairment to compare the health of adults nearing retirement by generation.9 They find that adults in their late 50s today are in poorer health than their parents’ generation was at the same age, even though the younger group will have to work longer to collect full Social Security benefits.
For this study, they used HRS and National Health Interview Survey (NHIS) data and divided older Americans into five groups based on the age at which they are eligible to collect full Social Security retirement benefits: those born in 1937 or earlier (age 65); those born 1938 to 1942 (between ages 65 and 66); those born 1943 to 1954 (age 66); those born 1955 to 1959 (between ages 66 and 67), and those born in 1960 to 1962 (age 67).
They find that the younger groups had higher shares of people who had at least one limitation on their ability to perform a basic daily living task by themselves, such walking across a room, dressing, bathing, eating, and transferring into or out of bed (see figure).
Also, they find that those born later tended to have higher rates of poor cognition, such as impaired memory and thinking ability, in their 50s compared with earlier generations at a similar age. Also, at age 50, people in the youngest group (born 1960 to 1962) were more likely to rate their own health as “fair” or “poor” than were people in the middle-three age groups when they were the same age, they report.
The researchers suggest that the increase of workers in their 50s and 60s who are in poor health will create significant challenges for them and their employers, including more people applying for Social Security disability payments. “Given the recent changes in health among the cohorts now approaching typical retirement age, further increases in the normal retirement age would place a substantial and disproportionate burden on these cohorts,” they argue.
The health of Americans in their 50s and early 60s today will shape labor force participation rates among the older population in the future. Understanding and monitoring these trends will be key as policymakers consider incentives to work longer and plan for future increases in the cost of public programs for older people.
Subscribe to our Today’s Research on Aging newsletter by sending an email to todaysresearch@prb.org with ‘Subscribe’ in the subject line.
1Courtney Coile, Kevin Milligan, and David Wise, “Health Capacity to Work at Older Ages: Evidence From the United States,” in Social Security Programs and Retirement Around the World: The Capacity to Work at Older Ages, National Bureau of Economic Research Conference Report, ed., David Wise (Chicago: University of Chicago Press, 2017).
2Hiram Beltrán-Sánchez, Marsha Jiménez, and S.V. Subramanian, “Assessing Morbidity Compression in Two Cohorts From the Health and Retirement Study,” Journal of Epidemiology and Community Health 70, no. 10 (2016): 1011-66.
3Eileen Crimmins, Yuan Zhang, and Yasuhiko Saito, “Trends Over Four Decades in Disability-Free Life Expectancy in the United States,” American Journal of Public Health 106, no. 7 (2016): 1287-93.
4Vicki Freedman et al., “Trends in Late-Life Activity Limitations in the United States: An Update From Five National Surveys,” Demography 49, no. 4 (2012).
5Linda G. Martin and Robert F. Schoeni, “Trends in Disability and Related Chronic Conditions Among the Forty-and-Over Population: 1997-2010,” Disability and Health Journal 7, no. 1 (2014): S4-14.
6HwaJung Choi, Robert Schoeni, and Linda G. Martin, “Are Functional and Activity Limitations Becoming More Prevalent among 55 to 69-Year-Olds in the United States?” PLoS One 11, no. 10 (2016): e0164565.
7Francesco Renna and Nidhi Thakur, “Direct and Indirect Effects of Obesity on U.S. Labor Market Outcomes of Older Working Age Adults,” Social Science & Medicine 71, no. 2 (2010): 405-13.
8National Center for Health Statistics (NCHS), “Prevalence of Obesity Among Adults and Youth: United States, 2015-2016” NCHS Data Brief, no. 288 (Oct. 2017).
9HwaJung Choi and Robert Schoeni, “Health of Americans Who Must Work Longer to Reach Social Security Retirement Age,” Health Affairs 36, no. 10 (2017): DOI 10.1377.
