Toshiko Kaneda
Technical Director, Demographic Research

Women spend more time as caregivers than men, and childless adults provide more support to their parents than those with children, studies on Europe show
September 8, 2023
Technical Director, Demographic Research
Europe is the oldest region in the world, with almost one in five people ages 65 and older . Many European countries are concerned about the implications of this aging population, including a growing demand for old-age support and a shrinking pool of working-age people to provide it. As the urgency of the care-work crunch becomes more apparent, new research funded by the National Institute on Aging reveals that women and people without children take on a disproportionate share of this unpaid care work across the continent.
Europeans can expect to spend over half of their lives after age 15 providing unpaid family care work, including taking care of children and older relatives. However, women in Europe spend six more years doing unpaid caregiving work than European men, according to a study by Ariane Ophir, now at the Center d’Estudis Demogràfics, and Jessica Polos, now at DePaul University. 1
Ophir and Polos estimated care life expectancy, or the number of years after age 15 people can expect to spend providing informal care, by sex in 23 European countries. 2 Data on unpaid caregiving came from the European Social Survey , and life expectancy data came from the Human Mortality Database’s abridged period life tables.
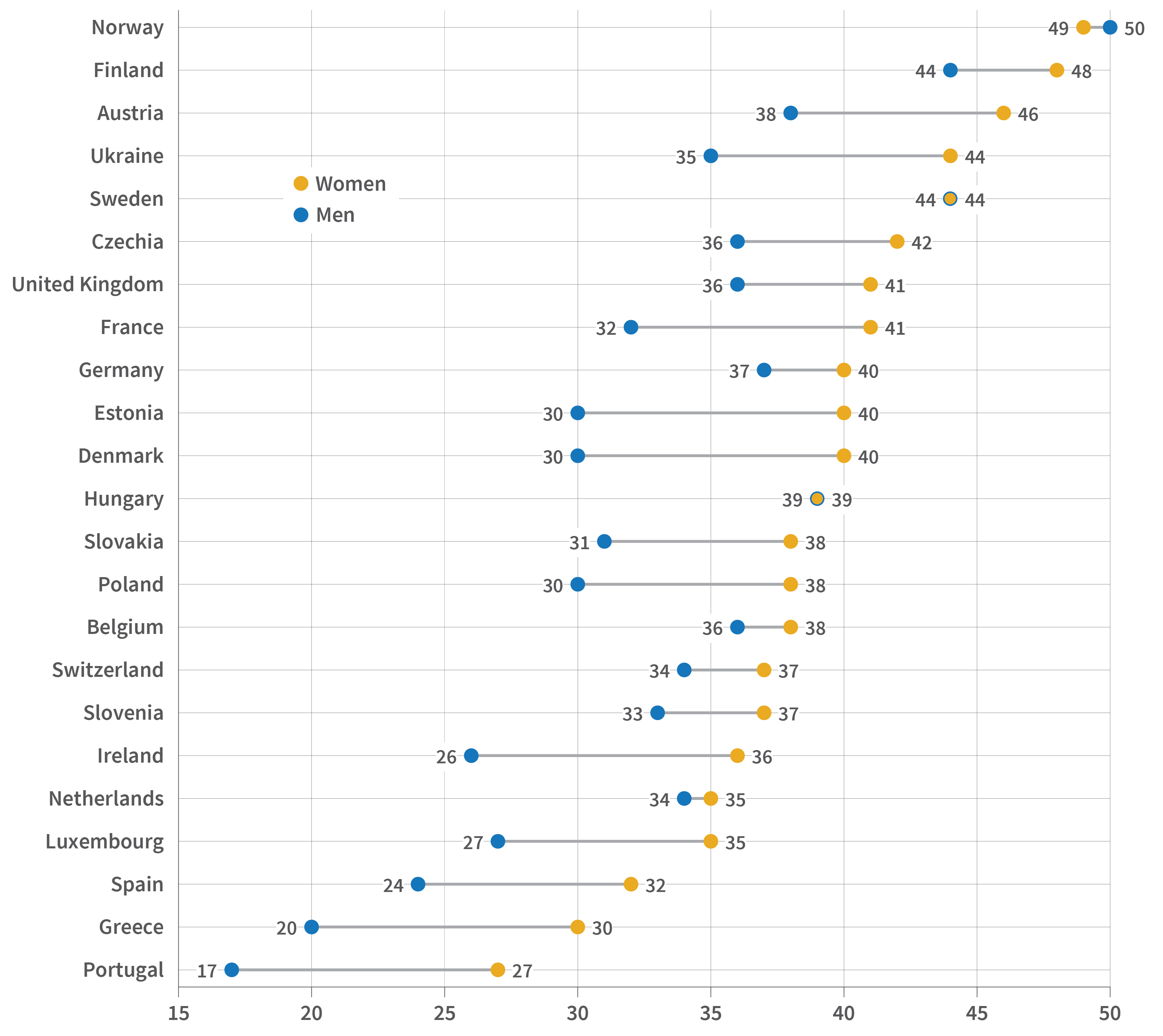
Source: Ariane Ophir and Jessica Polos, “Care Life Expectancy: Gender and Unpaid Work in the Context of Population Aging,” Population Research and Policy Review 41, no. 1 (2022): 197-227.
In the examined countries, the average care life expectancy is 33 years for men and 39 years for women, they found. And while the duration of caregiving life among men differs across countries—from 17 years in Portugal to 50 years in Norway—there is much less variability among women, reflecting how women consistently take on the primary caregiving burden, the authors explained.
By breaking down caregiving years by level of care, the authors also found that women spend significantly more time providing care at a high level, meaning daily or several times a week. In most of the examined countries, more than half of women’s caregiving years are spent on high-level care, compared to less than half of men’s. Women’s care life expectancy includes five to 10 more years of high-level caregiving than men’s in most countries, they found.
A similar gender gap in caregiving exists in the United States, according to Denys Dukhovnov of the University of California-Berkeley, Joan Ryan of the University of Pennsylvania, and Emilio Zagheni of the Max Planck Institute for Demographic Research.3 Compared to men who provide care, women spend 67% more time on average—around 50 minutes per day—providing unpaid care, their analysis found.
Using data from the American Time Use Survey and the Panel Study of Income Dynamics, Dukhovnov, Ryan, and Zagheni also showed that women in the United States spend twice as much time as men caring for young children, and that women in middle age spend slightly more time than men caring for older adults.
Both studies suggest the importance of considering the gender gap in informal caregiving when designing programs to promote more equitable work and family policies.
While women today are in the workforce longer than previous generations, they still spend fewer years employed than men in most European countries. But gender gaps in how long people work shrink or are even reversed when both paid and unpaid work are counted, a separate study by Ophir found.4
Ophir examined paid and unpaid working life expectancy at age 50 by sex, or the years 50-year-old women and men are expected to spend in employment and informal caregiving, including caring for grandchildren and helping older adults with daily activities. The study used data from the Survey of Health, Ageing, and Retirement in Europe (SHARE) from 17 countries across Europe.5
Women’s working life expectancy is longer than men’s by up to a year in all but four countries, but the components of this work are very different for men and women, the study found. The largest component for women is years spent exclusively in unpaid work, while for men it is years spent only in paid work. Women are also expected to spend more years than men simultaneously in paid and unpaid work in most countries, compounding their caregiving burden.
Most of the years women and men care for grandchildren occur after retirement, while some of the years they spend caring for older adults happen while still employed, especially for men, the study found. While women spend more years than men providing both types of care, the gap is larger with grandchild care, possibly reflecting women’s tendency to retire earlier, Ophir says.
Though concerns over the care burden in aging societies often focus on caring for older adults, caring for grandchildren is also an important part of working life among older women, Ophir says. Debates on increasing retirement age and work-family policies should therefore incorporate an intergenerational perspective, she suggests.
The gendered pattern of caregiving years suggests that women’s “additional investment in unpaid care work in older adulthood, which conflicts with paid work and does not count toward pension benefits, could exacerbate gender inequality later in life and expose older women to additional economic disadvantages,” Ophir further explains.
Luca Maria Pesando, now at New York University, found that adults with no children are about 20% to 40% more likely than those with children to provide financial, practical, and emotional support to their older parents, especially to mothers.6 Using Generations and Gender Survey (GGS) data from 11 European countries, his study examined support to older parents among adults ages 40 and older and whether having any children made a difference.7
Assessing the support provided to mothers and fathers separately also reveals gendered patterns. Women are more likely than men to provide support to mothers, regardless of whether they have children, Pesando found. Compared to those with children, both childless men and women are more likely to provide support to their mothers. In contrast, while childless women are more likely to provide support to their fathers, childlessness does not relate to the likelihood that men will provide support to their fathers.
The difference may reflect mothers being more socially and emotionally connected to their children than fathers, Pesando explains. Fathers are also more likely than mothers to have spouses still alive to provide support —reducing the potential burden on adult children—but the study controlled for this gender difference.
These findings are important in light of the growing share of childless adults in most European countries and concerns over the impact on demand for public support as people age. “These findings… support the view that researchers and policymakers should take into more consideration not only what childless people receive or need in old age, but also what they provide as middle-aged adults,” Pesando says.
While most countries in Europe older populations compared to the rest of the world, life expectancy and fertility levels vary. Norms around gender and family responsibilities also vary, partly reflecting differences in social policies that affect gender equality and care provision. All three studies conducted in Europe show variations in their findings across countries, in part due to their unique demographic profiles, norms, and policies.
Ophir and colleagues show that while the care life expectancy does not vary substantially across countries, the proportion of years spent providing high-level care differs. In Nordic countries such as Denmark and Sweden, women and men have longer care life expectancies but spend a smaller share of this time providing high-level care; they also have smaller gender gaps in caregiving. These countries have more egalitarian gender ideologies than other European countries and more generous welfare regimes that include family caregiving, the researchers say. They are also similar across some demographic factors, such as total fertility rate, age at first birth, life expectancy, and healthy life expectancy, they note.
In countries in Southern Europe, such as Greece, and some Central and Eastern European countries, such as Slovakia, care life expectancies are shorter but involve greater shares of high-level caregiving. These countries rely more on families to take on primary caregiving responsibilities, the researchers note. They do not, however, share similar demographic profiles, suggesting the importance of social contexts in addition to demographic factors in shaping the nature of care life expectancy, they add.
In her analysis examining both unpaid and paid work, Ophir also finds variation across countries in the intensity of care. For example, while the overall working life expectancy is the longest for Swedish adults, most of their unpaid work was low intensity, reflecting the country’s generous welfare regime. While the overall working life expectancy is relatively shorter in Greece, Italy, and Poland, most of the unpaid work for women involves higher-level caregiving.
Pesando finds that adults are less likely to care for their older parents in Northern Europe, where comprehensive publicly funded programs can provide this care. Though differences are not large among countries in Eastern and Western Europe, adults are most likely to support older parents in Russia, followed by Czechia. Both countries are former socialist welfare states with heavy reliance on family support and limited publicly funded services for older adults, he notes.
Despite concerns over the economic implications of population aging and the labor force participation of older adults, informal caregiving has received little attention in policy debates. The disproportionate burden that falls on women and adults without children is therefore largely unnoticed. Discussions of aging-related policies, including pension reforms, old-age entitlements, and changes in the retirement age, should be informed by patterns in informal caregiving. Addressing informal caregiving also helps promote gender equality, especially in later life.
