Today’s Research on Aging, No. 42 (2022)

BOX
Obesity in Midlife Is Linked to Increased Risk of Dementia
Obesity’s role in dementia risk has puzzled researchers: Some studies show that obesity in midlife (between ages 40 and 60) is linked to lower cognitive function and increased dementia risk in old age. But obesity after age 65 appears to provide some protection from dementia, while being underweight at older ages raises dementia risk, reports Kenneth Langa and colleagues based on nationally representative U.S. Health and Retirement Study (HRS) data. One theory is that being overweight or obese at older ages might provide buffering reserves of muscle and fat that slow the progression of chronic disease, while unintentional weight loss may be an early sign of dementia onset. Another theory suggests that the link between being underweight and developing dementia is so strong that people with obesity appear to be protected from dementia.
Ida Karlsson and colleagues also analyzed a related set of HRS data and noted the link between being underweight and having dementia. But they also find a strong connection between higher BMI and declining cognitive abilities throughout both midlife and late life, especially among men and individuals with genes that predispose them to a low BMI. Similarly, a recent study based on data from the English Longitudinal Study of Ageing shows that overweight or obese older adults were more likely than their peers to develop dementia 11 years later. Women face a higher dementia risk than men related to their having central obesity (high waist circumference). In addition, the study finds that the association between obesity and dementia is independent of whether a person was a smoker, had hypertension or diabetes, or carried the APOE ε4 gene, a genetic risk factor for Alzheimer’s disease and related dementias.

References
1 Federal Interagency Forum on Aging-Related Statistics, Older Americans 2020: Key Indicators of Well-Being (Washington, DC: U.S. Government Printing Office, 2020). Percentage of people ages 65 and over who are overweight and have obesity, by sex and age group, selected years, 1976-2018.
2 U.S. Centers for Disease Control and Prevention (CDC), “Adult BMI Calculator.”
3 Craig M. Hales et al., “Prevalence of Obesity and Severe Obesity Among Adults: United States,
2017-2018,” NCHS Data Brief, no. 360 (Hyattsville, MD: National Center for Health Statistics, 2020).
4 CDC, “Obesity, Race/Ethnicity, and COVID-19.”
5 Samuel H. Preston, Yana C. Vierboom, and Andrew Stokes, “The Role of Obesity in Exceptionally Slow U.S. Mortality Improvement,” Proceedings of the National Academy of Sciences of the United States of America 115, no. 5 (2018): 957-61.
6 Morgan E. Levine and Eileen M. Crimmins, “Is 60 the New 50? Examining Changes in Biological Age Over the Past Two Decades,” Demography 55, no. 2 (2018): 387-402.
7 Kaitlyn M. Berry, et al., “Association of Weight at Different Ages and All-Cause Mortality Among Older Adults in the U.S.,” Journal of Aging and Health (2022): 1-15.
8 Tarlise N. Townsend and Neil K. Mehta, “Contributions of Obesity and Cigarette Smoking to Incident Disability: A Longitudinal Analysis,” Preventive Medicine 141 (2020): 106226.
9 Andrew C. Stokes et al., “Increases in BMI and Chronic Pain for U.S. Adults in Midlife, 1992 to 2016,” SSM – Population Health 12 (2020): 100644.
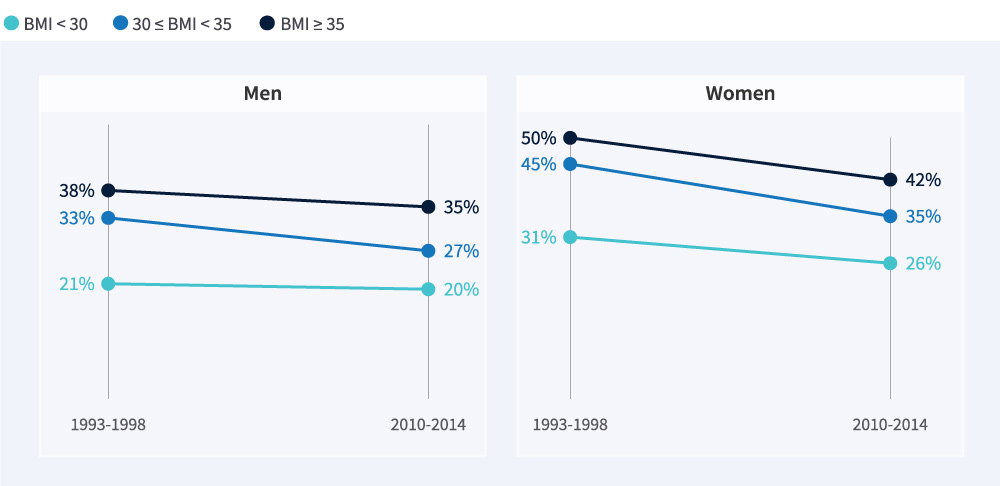
10 Jung Ki Kim, Jennifer A. Ailshire, and Eileen M. Crimmins, “Twenty-Year Trends in Cardiovascular Risk Among Men and Women in the United States,” Aging Clinical and Experimental Research 31, no. 1 (2019): 135-43.
11 Yuan S. Zhang, Yasuhiko Saito, and Eileen M. Crimmins, “Changing Impact of Obesity on Active Life Expectancy of Older Americans,” Journals of Gerontology, Series A: Biological Sciences and Medical Sciences 74, no. 12 (2019): 1944-51.
12 Peter Hudomiet, Michael D. Hurd, and Susann Rohwedder, “Trends in Health in Midlife and Late Life,” Journal of Human Capital 16, no. 1 (2022).
13 Irma T. Elo, Neil Mehta, and Samuel Preston, “The Contribution of Weight Status to Black-White Differences in Mortality,” Biodemography and Social Biology 63, no. 3 (2017): 206-20, doi:10.1080/19485565.2017.1300519. 29035108.
14 Yang Claire Yang et al., “Life-Course Trajectories of Body Mass Index From Adolescence to Old
Age: Racial and Educational Disparities,” Proceedings of the National Academy of Sciences of the United States of America 118, no. 17 (2021): e2020167118, doi:10.1073/pnas.2020167118.
15 Roland J. Thorpe, Jr., “Association Between Discrimination and Obesity in African-American Men,”Biodemography and Social Biology 63, no. 3 (2017): 253-61, doi:10.1080/19485565.2017.1353406.29035104.
16 Steven W. Cole et al., “Population-Based RNA Profiling in Add Health Finds Social Disparities in Inflammatory and Antiviral Gene Regulation to Emerge by Young Adulthood,” Proceedings of the National Academy of Sciences of the United States of America 117, no. 9 (2020): 4601-08, doi:10.1073/pnas.1821367117.
17 Daniel Parker et al., “Age-Related Adverse Inflammatory and Metabolic Changes Begin Early in Adulthood,” The Journals of Gerontology: Series A, Biological Sciences and Medical Sciences 74, no. 3 (2019): 283-9, doi:10.1093/gerona/gly121.
18 Michael J. A. Williams et al., “Childhood Body Mass Index and Endothelial Dysfunction Evaluated by Peripheral Arterial Tonometry in Early Midlife,” International Journal of Obesity 41, no. 9 (2017): 1355-60, doi:10.1038/ijo.2017.108.
19 Jessica J. Chiang et al., “Adiposity Moderates Links From Early Adversity and Depressive Symptoms to Inflammatory Reactivity to Acute Stress During Late Adolescence,” Brain, Behavior, and Immunity 66 (2017): 146-55, doi:10.1016/j.bbi.2017.06.015.
20 Alexander M. Kulminski et al., “Independent Associations of TOMM40 and APOE Variants With Body Mass Index,” Aging Cell 18, no. 1 (2019): e12869, doi:10.1111/acel.12869.
21 Karri Silventoinen et al., “Differences in Genetic and Environmental Variation in Adult BMI by Sex, Age, Time Period, and Region: An Individual-Based Pooled Analysis of 40 Twin Cohorts,” American Journal of Clinical Nutrition 106, no. 2 (2017): 457-66, doi:10.3945/ajcn.117.153643.
22 Michael J. Parsons et al., “Social Jetlag, Obesity and Metabolic Disorder: Investigation in a Cohort Study,” International Journal of Obesity 35, no. 5 (2015): 842-8, doi:10.1038/ijo.2014.201.
23 John Cawley et al., “Direct Medical Costs of Obesity in the United States and the Most Populous States,” Journal of Managed Care & Specialty Pharmacy 27, no. 3 (2021): 354-66.
24 Claire K. Ankuda et al., “Caregiving for Older Adults with Obesity in the United States,” Journal of the American Geriatrics Society 65, no. 9 (2017): 1939-45, doi:10.1111/jgs.14918.
25 John A. Harris et al., “The Relationship of Obesity to Hospice Use and Expenditures: A Cohort Study,” Annals of Internal Medicine 166, no. 6 (2017): 381-9, doi:10.7326/M16-0749.
26 Peter Hudomiet, Michael D. Hurd, and Susann Rohwedder, “Forecasting Mortality Inequalities in the U.S. Based on Trends in Midlife Health,” Journal of Health Economics 80, (2021): 102540.
27 Iliya Gutin, “Educational Differences in Mortality Associated With Central Obesity: Decomposing the Contribution of Risk and Prevalence,” Social Science Research 90 (2020): 102445, doi:10.1016/j.ssresearch.2020.102445.
28 Barry M. Popkin et al., “Towards Unified and Impactful Policies to Reduce Ultra-Processed Food Consumption and Promote Healthier Eating,” Lancet Diabetes Endocrinology 9, no. 7 (2021): 462-70, doi:10.1016/S2213-8587(21)00078-4; Tadeja Gračner, “Bittersweet: How Prices of Sugar-Rich Foods Contribute to the Diet-Related Disease Epidemic in Mexico,” Journal of Health Economics 80 (2021): 102506; Andrea S. Richardson et al., “Obesity Prevention Interventions and Implications for Energy Balance in the United States and Mexico, A Systematic Review of the Evidence and Meta-Analysis,” Obesity 27, no. 9 (2019): 1390-1403, doi:10.1002/oby.22540.
29 Patricia M. Herman, PhuongGiang Nguyen, and Roland Sturm, “Diet Quality Improvement and 30-Year Population Health and Economic Outcomes: A Microsimulation Study,” Public Health Nutrition, 13 (2021): 1-9.
30 Hilary Hoynes, Diane Whitmore Schanzenbach, and Douglas Almond, “Long Run Impacts of Childhood Access to the Safety Net,” American Economic Review 106, no. 4 (2016): 903-34.
31 Wubin Xie et al., “Association of Weight Loss between Early Adulthood and Midlife with All-Cause Mortality Risk in the U.S.,” JAMA Network Open 3, no. 8 (2020): e2013448.



 ">
">