Date
December 19, 2025
English Publication
The Demographics of African Faculty in the East African Community (DAF-EAC) is a study undertaken by a consortium comprised of the Inter-University Council for East Africa (IUCEA), Education Sub Saharan Africa (ESSA), the Association of African Universities (AAU), and the Population Reference Bureau (PRB). DAF-EAC follows the initial study on Demographics of African Faculty in Ghana, which provided important demographic data and identified challenges concerning faculty in the country.
DAF-EAC sought to assess the status of Higher Education faculty in the East African region in terms of numbers, distribution by gender and areas of study. The study comprised four components namely; background research, analysis of current and future faculty demand, stakeholder engagement and dissemination of study findings, and co-creation of solutions to address the faculty challenges. The study was funded by the Carnegie Corporation of New York (grant number G-21-58066), focusing on six Partner States of the East African Community, namely Burundi, Kenya, Rwanda, South Sudan, Tanzania, and Uganda.

Date
October 30, 2025
English Publication
Higher education data management covers a broad range of information, including students, faculty, other staff, research and development, facilities, and financial resources. This document presents two complementary sets of indicators—student indicators and faculty indicators—designed to support consistent data collection and analysis within higher education systems. These indicators are intended to inform planning, monitoring, and decision-making, with a particular emphasis on understanding and addressing faculty staffing needs, a core objective of the Demographics of African Faculty (DAF) project.

New Data Reveal Appalachia’s Economic Improvements, Key Vulnerabilities Compared to the Rest of the U.S. Economy
Report from ARC and PRB finds decreased unemployment, increased labor force participation, and higher homeownership in Appalachia—but the Region still lags behind the U.S. in population and income growth, as well as post-secondary education attainment.
Date
July 3, 2025
Sara Srygley
Research Associate
Nurfadila Khairunnisa
Research Analyst
Diana Elliott
Senior Vice President, Programs
Download Chartbook
Focus Area
New data released by the Appalachian Regional Commission (ARC) and PRB in the 15th annual update of The Appalachian Region: A Data Overview from the 2019-2023 American Community Survey shows that rates of labor force participation and homeownership continue to improve in Appalachia.
Drawing from the latest American Community Survey and comparable 2023 Census Population Estimates, the report, known as “The Chartbook,” contains more than 300,000 data points comparing Appalachia’s regional, subregional and state data with the rest of the nation.
Key improvements in the region’s economic indicators are as follows:
Decrease in unemployment rates and higher labor force participation
- Appalachia’s unemployment rate decreased by 0.8 percentage points between 2014-2018 to 2019-2023, compared to a 0.4 percentage point decrease in the rest of the U.S.
- Appalachia’s labor force participation rate among civilians ages 25 to 64 was 1.5 percentage points higher in 2019-2023 than it was in 2014-2018, slightly outpacing the national increase of 1.2 points.
Homeownership bypasses national average
- Among occupied housing units, homeownership in the region was 6.7 percentage points higher than in the U.S. overall.
- However, housing unit vacancy in the Appalachian Region was 3.4 percentage points higher than the national average.
Below average number of cost burdened households
- The share of households in Appalachia that are cost burdened – where housing costs are 30% or more of monthly income—is 6.7 percentage points lower than the U.S. average.
- In Appalachia and nationally, housing cost burden is highest among the youngest and oldest renters.
“While Appalachia continues to make progress toward reaching economic parity with the rest of the country, it’s important to recognize there is still work to be done,” said ARC Federal Co-Chair Gayle Manchin. “ARC will continue to partner on the local, state, and federal levels to prioritize the future of Appalachia’s 13 states and remains committed to ensuring Appalachians have access to the education, job training and infrastructure they need for prosperous lives in the places they love.”
“This year’s Chartbook highlights important economic advances, not only in Maryland but across the Appalachian Region—including gains in employment and homeownership,” said ARC 2025 States’ Co-Chair, Maryland Governor Wes Moore. “By working together, we continue to uplift our most vulnerable populations, promoting a better, brighter future for all families across Appalachia.”
Despite positive trends, several data points revealed key challenges affecting Appalachian economies compared to the rest of the nation:
Despite population increase, growth lags
- Appalachia’s population is growing – but more slowly than the nation as a whole.
- Growth in the region was 4.3 percentage points lower than the national average between 2010 and 2023.
- In addition, Appalachia’s population is, on average, 2.2 years older than the U.S. population, with 1 in 5 Appalachian residents age 65 or older.
Post-secondary educational attainment remains behind national average
- 27.3% of Appalachians hold a bachelor’s degree or higher, falling behind the national average of 35%.
Greater share of Appalachians live in poverty
- At $64,588, the median household income in Appalachia is nearly $14,000 below the U.S. average of $78,538.
- More than 14% of Appalachians live in poverty or “deep” poverty.
“The data point to bright spots but also guide us to areas where targeted efforts could improve well-being for Appalachians across the region,” said Sara Srygley, a senior research associate at PRB. “Decisionmakers and advocates can use the Chartbook to create the changes they want to see in their communities.”
The data shows that Appalachia’s rural areas continue to be at increased risk for economic distress compared to its urban areas. Appalachia’s 107 rural counties are also more uniquely challenged, compared to 841 similarly designated rural counties across the rest of the U.S., as rural Appalachian counties continue to lag behind on indicators including educational attainment and household income.
The data also highlights key differences between Appalachia’s subregions, including:
- Northern Appalachia has the highest share of adults with a bachelor’s degree or more in the science and engineering field at 32.4%.
- North Central Appalachia has the highest share of veterans among the subregions.
- Central Appalachia saw an increase in digital device ownership and internet access, although broadband access remains a challenge.
- South Central Appalachia experienced one of the most significant decreases in cost-burdened households compared to other subregions.
- Southern Appalachia has the highest mean and median incomes—and income per capita is increasing more than in the other subregions.
In addition to the written report co-authored by the Population Reference Bureau, ARC offers companion web pages on Appalachia’s population, employment, education, income and poverty, computer and broadband access, and rural Appalachian counties compared to the rest of rural America’s counties. For more information, visit www.arc.gov/chartbook.
About the Appalachian Regional Commission
The Appalachian Regional Commission is an economic development entity of the federal government and 13 state governments focusing on 423 counties across the Appalachian Region. ARC’s mission is to innovate, partner, and invest to build community capacity and strengthen economic growth in Appalachia to help the region achieve socioeconomic parity with the nation.

Collaborating for Action on the Future of Demographic and Health Surveys
This convening held on May 7-8, 2025, brought together key stakeholders—including leaders from National Statistical Offices, donor organizations, partner organizations, and data user groups—to identify opportunities and priorities for collaboration to protect current data and preserve ongoing data collection activities.
Date
June 25, 2025
Meeting Report
Since 1984, USAID has funded the Demographic and Health Surveys (DHS) Program to provide technical assistance to more than 400 surveys in over 90 countries. On February 24, 2025, the U.S. government terminated the DHS Program. In the aftermath of the termination, numerous efforts have emerged to mobilize action to sustain collection of high-quality demographic and health data through surveys. These efforts span a range of critical challenges, including preservation and accessibility of current data, completion of near-final surveys, and identifying long-term strategies to support future data collection. As multiple streams of effort have emerged, PRB organized a virtual global convening to support coordination and collaboration.
The convening brought together key stakeholders—including leaders from National Statistical Offices, donor organizations, partner organizations, and data user groups—to identify opportunities and priorities for collaboration to protect current data and preserve ongoing data collection activities. This event created a space to identify needs, gaps, opportunities, and emerging solutions; share efforts that are underway; and support ongoing coordination among stakeholders moving forward.
This meeting report summarizes the discussion and ideas shared in the convening. Each topic, objective, and related stakeholder discussion is presented, with little interpretation, to form a record of the conversation and ideas that arose. This report concludes with a summary of emerging next steps.
For questions about the report or to learn more about ways to engage ongoing dialogue on the future of the DHS, contact Kaitlyn Patierno (kpatierno@prb.org).

Date
March 18, 2025
English Publication
In June 2024, the MOMENTUM Knowledge Accelerator Project, FP2030, and the William H. Gates Sr. Institute for Population and Reproductive Health at the Johns Hopkins Bloomberg School of Public Health (the Organizing Committee) jointly hosted a convening, “Centering Locally-Driven Family Planning Measurement Priorities in the Global Measurement Agenda,” in Nairobi, Kenya. Funded by the U.S. Agency for International Development (USAID) and the Bill & Melinda Gates Foundation, the convening aimed to elevate the voices of country-based family planning (FP) actors in the global FP measurement discourse. From June 25–27, over 50 program implementers, monitoring and evaluation (M&E) officers, statistical officers, and local researchers from 22 countries came together to discuss challenges, gaps, emerging approaches, and technical assistance needs in FP measurement at the global, national, subnational, and community levels. The Nairobi convening is designed to serve as a launch-point for an ongoing effort to advance FP measurement through multidirectional learning and exchange between country and global stakeholders, the FP Measurement Advancement Convening Series, or “FP-MACS.”

Date
January 15, 2025
English Publication
PRB created The KIDS COUNT Data Resource Guide to facilitate the use of population data from the U.S. federal statistical system. Originally designed for the KIDS COUNT program on child well-being, the guide offers practical advice on how to use major data sources—from the Decennial U.S. Census to the National Vital Statistics System—that could be helpful to anyone who works with U.S. population data.
The guide includes an overview of each major data source, including what data are available, how to access that data, and some best practices for using each source. These sources provide up-to-date and reliable information that is comparable across all 50 states, the District of Columbia, and, where available, Puerto Rico and the U.S. Virgin Islands.
Data sources covered by the guide include:
- Decennial Census
- U.S. Census Bureau Population Estimates Program
- American Community Survey
- Current Population Survey
- National Vital Statistics System
- National Survey of Children’s Health
- Small Area Income and Poverty Estimates
- Small Area Health Insurance Estimates
- National Center for Education Statistics
- And more
The KIDS COUNT Data Resource Guide also includes a brief overview of best practices that apply across data sources, such as assessing reliability, making comparisons, and disaggregating by race and ethnicity.

Research Technical Assistance Center
Date
December 30, 2024
English Publication
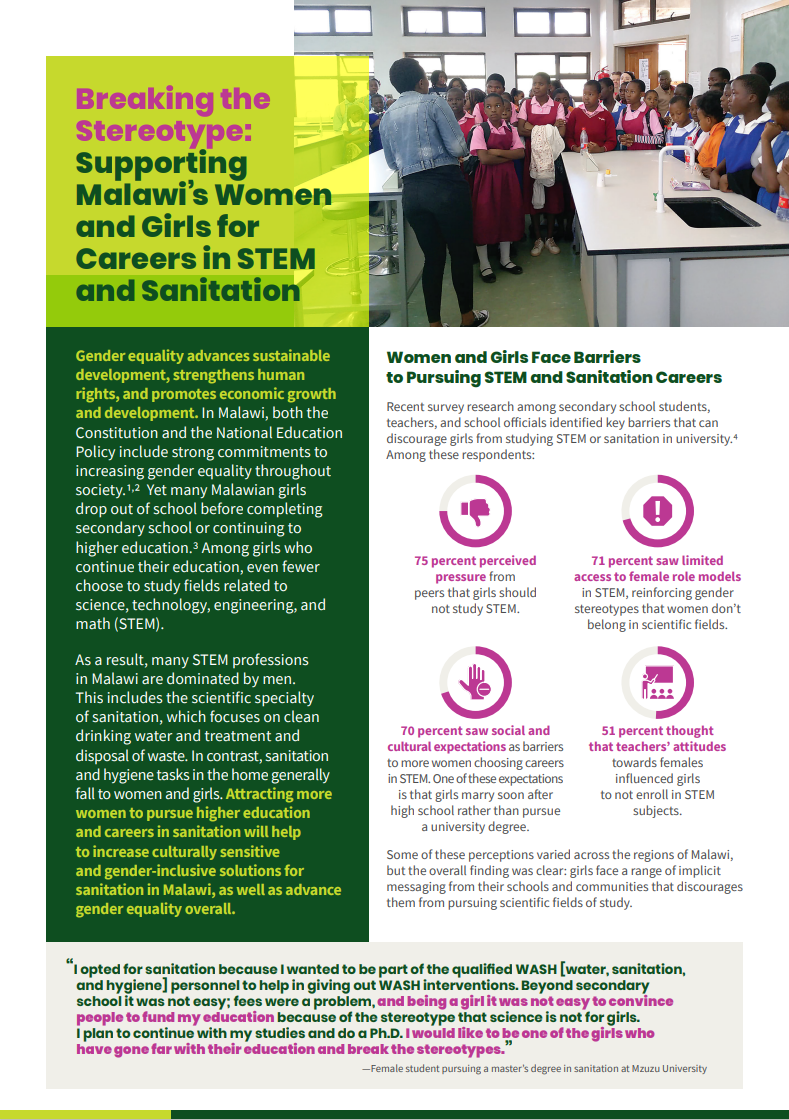
Gender equality advances sustainable development, strengthens human rights, and promotes economic growth and development. Even with commitments made by the Government of Malawi to increase gender equality throughout society, many Malawian girls drop out of school before completing secondary school or continuing to higher education. Among those who remain, even fewer chose to study in fields related to STEM and sanitation. As a result, many STEM and sanitation professions in Malawi are dominated by men, even though sanitation and hygiene tasks in the home general fall to the women and girls. This factsheet shares recent survey research from Mzuzu University and explains how attracting more women to pursue higher education and careers in sanitation will help to increase culturally sensitive and gender-inclusive solutions for sanitation in Malawi, as well as advance gender equality overall.
Research Technical Assistance Center
Date
December 30, 2024
English Publication
Researchers from the University of Liberia College of Health Sciences, in partnership with the University of Michigan School of Nursing and the Kwame Nkrumah University of Science and Technology, developed and tested a mobile obstetric emergency system (MORES) that reduced decision-to-delivery time in Bong County, Liberia, shortening the time between the decision to perform an emergency surgical birth and delivery of the newborn. By improving communication among health workers during obstetric triage with WhatsApp, a mobile messaging service, a MORES can help prevent deaths from emergencies related to pregnancy and childbirth.
This brief provides additional information on cesareans and triage and how better communication can be lifesaving for mothers and newborns. In addition to sharing details of the research and an example of closed-loop communication system at work, the brief provides two recommendations for the Liberian Ministry of Health to reduce decision-to-delivery times and improve perinatal outcomes, thereby saving lives.

Research Technical Assistance Center
Climate change has wide-ranging effects on farming communities throughout the world, as unpredictable weather patterns cause irregular rainfall and destabilize longstanding agricultural practices. In Bhutan’s Pemagatshel District, climate change is compromising food ecosystems and escalating conflict between humans and wildlife. Nearly half of the district’s residents are small-scale farmers who depend on agriculture for their livelihoods and are highly vulnerable to the effects of climate change.
To help address these affects, new research from Royal University of Bhutan and the University of Montana examined how adopting climate-smart agriculture in small-scale farming practices can help mitigate the negative effects by improving food production and food security. This brief shares provides additional background on Pemagatshel’s farming practices and climate-smart agriculture and shares how the key research findings reveal promising opportunities. The brief concludes with three recommended actions to protect Bhutan’s small-scale farmers from climate change.
This brief is available in English and Dzongkha.
Quick Links

PUBLICATION
Today’s Research on Aging, No. 44 (2024)
AUTHORS
Paola Scommegna
Contributing Senior Writer
Mark Mather
Associate Vice President, U.S. Programs
Diana Elliott
Senior Vice President, Programs
PRINT PUBLICATION
Older Americans with strong social connections are healthier and live longer than their socially isolated peers. Increasingly, researchers are finding that the components of good health are not only the absence of mental disorders and physical disease but also the presence of robust social relationships.
This brief explores recent research probing the dynamics of social connection and health supported by the National Institute on Aging. The findings point to myriad ways in which social ties bolster health—from slowing aging and boosting cancer-fighting hormones to preventing depression and protecting memory. Health policymakers and program planners can use this evidence to inform a variety of interventions—particularly those aimed at reducing social isolation in vulnerable groups—to support longer and healthier lives for older Americans.
Strong Social Ties Slow Aging, Lower Risk of Death
Studies have shown that both the quality and quantity of our social ties shape our mental and physical health, health behaviors, and mortality risk. Researchers are studying multiple aspects of our social lives—from the levels of social support we receive to our activities and the strength of our social networks—to understand how they link to health outcomes.
Healthy, supportive relationships with family and friends may slow aging, concluded a research team from the University of California, Los Angeles (UCLA) and the University of Southern California (USC).1 According to their DNA, older adults with the most supportive relationships with spouses, adult children, other family members, and friends were aging one to two years slower than those who lacked such ties, they found. The pace of such aging is important—rapid epigenetic aging at younger chronological ages can contribute to the early onset of chronic disease and disability and premature death.

The healthiest older adults had strong social connections and just a 4% risk of dying within five years.
The authors, led by Kelly E. Rentscher, based their analysis on aging-related molecular changes in DNA among older adults participating in the nationally representative Health and Retirement Study (HRS). Even after factoring in smoking, alcohol use, and other lifestyle factors known to accelerate aging, the protective role of strong social relationships persisted, they reported.
Supportive relationships with spouses and children helped slow the pace of aging by more than three weeks per year, they found. Having support from other family members and friends also helped slow the pace of aging, by about three weeks per year and more than two weeks per year, respectively.
Older adults with the most supportive relationships were aging one to two years slower than those who lacked such ties.
Overall, the findings affirm that both the presence of relationships and their quality mattered for longevity. The new study may support interventions with the potential to “prevent, slow, or reverse accelerated aging and extend the healthspan and lifespan,” the authors wrote.
Other ongoing research underscores the important role of social factors in the overall health of older adults. Linda Waite and Yiang Li from the University of Chicago found that the healthiest older adults had strong social connections and just a 4% risk of dying within five years, while those with the poorest health had weaker social connections and a 57% risk of dying within five years.2 Key factors linked to longevity included robust social networks and partnered sexual activity, highlighting the importance of social integration in maintaining health in later life. Their preliminary findings are based on nationally representative data from the National Social Life, Health, and Aging Project (NSHAP).
Social Connections May Improve the Well-Being of Patients With Cancer and Other Health Conditions
More new research poses that social connections may also improve the well-being of cancer patients by boosting protective hormones.
A research team from six major universities found that in ovarian cancer patients, social support was associated with higher levels of oxytocin—a hormone linked to some protection against cancer.3 Specifically, having a more positive outlook, a sense of purpose, and a role in caring for others at the time of cancer surgery were associated with higher oxytocin levels. (However, a person’s perceived closeness with others was not related to higher oxytocin levels.)
“Nurturance is consistent with the oxytocin-focused ‘tend and befriend’ hypothesis of female coping and stress response,” wrote the team, led by Michaela G. Cuneo at the University of Iowa. Thus, even though this research is in the early stages, feeling needed by others could have protective health effects for women with ovarian cancer.
Similarly, another team of researchers at the National Cancer Institute and the University of Wisconsin–Madison found that strong, supportive relationships between cancer patients and their caregivers were associated with better self-reported health for both parties.4 This was especially the case for those dealing with lung cancer, where social support was linked to better self-reported health 12 months after diagnosis. Dannielle E. Kelley and coauthors speculate that there may be a beneficial “partner effect” for lung cancer that can counter internalized and social stigmas associated with the disease for former smokers.

Strong, supportive relationships between cancer patients and their caregivers were associated with better self-reported health for both parties.
Social connections might also help a patient adopt more healthful behaviors after diagnosis—but the benefits could depend on their education level. According to Won-tak Joo of the University of Florida, college graduates have more robust health conversations with people in their social networks at the time of diagnosis, which may help explain why they are more successful at improving their health behaviors and show a better prognosis than those with lower education levels.5
“The cultivation of health discussion may be more active in earlier stages of illness when patients require external support to adapt to new lives with diseases,” writes Joo. For older adults with lower levels of education, Joo finds that both social networks and health conversations decline with disease diagnosis, suggesting a need for interventions to help this group.
Researchers are also studying how social ties affect the health of older people with disabilities. Karen L. Fingerman of the University of Texas at Austin and colleagues find that those with limiting disabilities were more likely to attend medical appointments when spending time with friends and family.6 And Sophie Mitra of Fordham University and coauthors report that older adults with disabilities have as much close, regular contact with partners, family, and friends as those without disabilities.7 For those with disabilities and others with serious medical conditions, social connectedness may lead to help with activities that improve their health and well-being.
Connectedness also affects our health in ways that ultimately impact our sleep. A recent study from China’s Xi’an Jiaotong University, the University of Texas at Austin, and the University of Maryland found that socially isolated older adults—those with smaller and less intimate relationships—had more depressive symptoms, were lonelier, and had more chronic diseases and pain, all of which contributed to greater sleep difficulty.8 Dan Zhang and coauthors argue that improving older adults’ social connections could enhance their mental, physical, and sleep health.
A Lifetime of Experiences Shape Social Connections at Older Ages
Some groups of people are more likely to be socially isolated than others, report Debra Umberson of the University of Texas at Austin and Rachel Donnelly of Vanderbilt University.9 Older married women may become socially isolated when a spouse needs round-the-clock care, while men who either never marry or divorce may begin experiencing social isolation in young adulthood.
In addition, non-Hispanic Black and Hispanic older adults are more likely to experience social isolation than non-Hispanic older white adults, they found (see Figure 1). Black and Hispanic Americans’ social isolation could be related to the impact of lifetime discrimination and financial stress, the researchers suggest. Using HRS data, the study measured isolation among adults ages 50 and older based on whether they are married or cohabiting, participate in volunteer activities, and have contact with parents, children, and neighbors.
Figure 1. Older Non-Hispanic Black Americans Experience Higher Levels of Social Isolation Than Other Groups
Mean Levels of Social Isolation Among U.S. Adults Ages 50 and Older in the Health and Retirement Study, by Race/Ethnicity
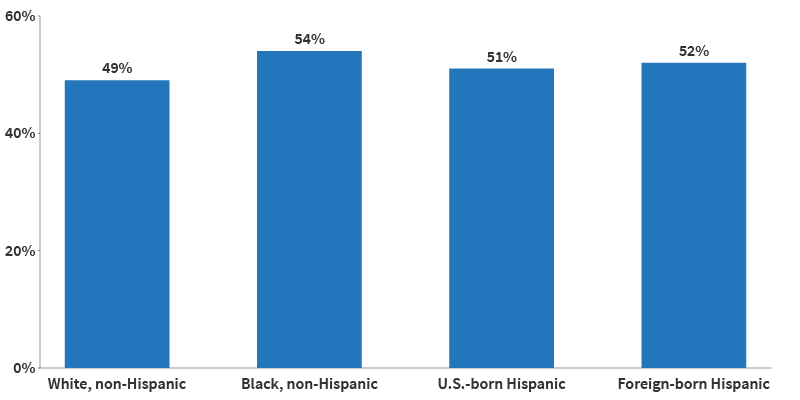
Source: Debra Umberson and Rachel Donnelly, “Social Isolation: An Unequally Distributed Health Hazard,” Annual Review of Sociology 49, no. 1 (2023): 379-99.
Another study out of Johns Hopkins University estimated that nearly one in four (24%) of older Americans living in the community are socially isolated, and one in 25 (4%) are severely isolated.10 To measure isolation, they examined participants’ living arrangements, religious attendance, social activities, and the number of people they spoke with about important matters. The study used data from the National Health and Aging Trends Study, which includes a nationally representative sample of Medicare beneficiaries ages 65 and older.
Being unmarried, male, and having low education and income levels increased the odds of being socially isolated, according to the analysis, led by Thomas Cudjoe. Specifically, men were four times as likely as women to be severely isolated, while people with annual incomes below $30,000 were twice as likely as people with incomes over $60,000 to be severely isolated. These findings offer “easily identifiable” factors to help program planners target those most at risk, the researchers wrote, noting that living arrangements, discussion networks, and social activities can all be modified to improve social connections.
Calling social isolation “an unequally distributed health hazard,” Umberson and Donnelly urge future researchers to undertake “a systematic assessment of social conditions that foster isolation over the life course” to better understand the root causes and identify ways to reduce isolation among those most at risk.
Being unmarried, male, and having low education and income levels increased the odds of being socially isolated.
“We need to understand why people become more isolated over their lives, because social isolation is a public health issue,” Umberson said. “People became more concerned about isolation in the wake of Covid-19 because we were all more isolated for several years, but this is a problem that’s likely to become more serious, not less.”11
The stability of older adults’ lives may also contribute to richer social networks. While younger adults experienced turnover in social networks after a major life transition, such as getting married or having children, older adults maintained relatively stable social networks after such changes, including retirement, changes in marital status, or becoming empty nesters, found Jordan Weiss and team at the University of California, Berkeley.12 The authors suggest that for older adults, having stable, long-term (often decades-old) relationships make for more reliable networks.
A person’s temperament also may influence their lifelong social ties. Using NSHAP data, James Iveniuk at the University of Toronto finds that among older Americans, personality traits such as extraversion and agreeableness were associated with stronger social ties than openness, conscientiousness, or neuroticism.13 Thus, certain personality traits may strengthen the social connections linked to health benefits.
Social Networks May Protect Mental Health and Prevent Cognitive Decline
Older adults’ social networks may protect both their mental health and cognitive abilities. Getting help with daily activities may be an important reason why—since many older adults need assistance bathing, getting in and out of bed, and doing other tasks, some built-in social interaction can accompany aging. But feelings of closeness and companionship may also help stave off memory loss, loneliness, and depression—and may matter as much or more than geographic proximity or number of family or friends, new research shows.
To try to understand the importance of relationship quality, Sarah Patterson of the University of Michigan and Rachel Margolis of the University of Western Ontario looked at four groups of older adults with different types of family connections: those who were geographically and emotionally close with family; those who were kinless and without a partner or children; those who were distanced and lived far from family; and those who were disconnected and had no family members in their social network or did not know where they lived.14

The closeness of the relationships—especially with family—buffered loneliness.
“We were interested in understanding how much the presence of family ties matters for older adults’ well-being but also in measuring the quality of those relationship ties,” said Patterson.15
They found that older adults who lived near family members and discussed important concerns with them were less likely to report unmet need for help with daily activities than the other groups (see Figure 2). Meanwhile, those who reported no partner or family or disconnection had the poorest mental health and socialized less often—even less than those who lived far away from their family.
Figure 2. Older Adults Who Are Close to Family Get More Help With Activities
Share of adults ages 70 and older reporting unmet need for help with activities by type of family connections, 2015–2019
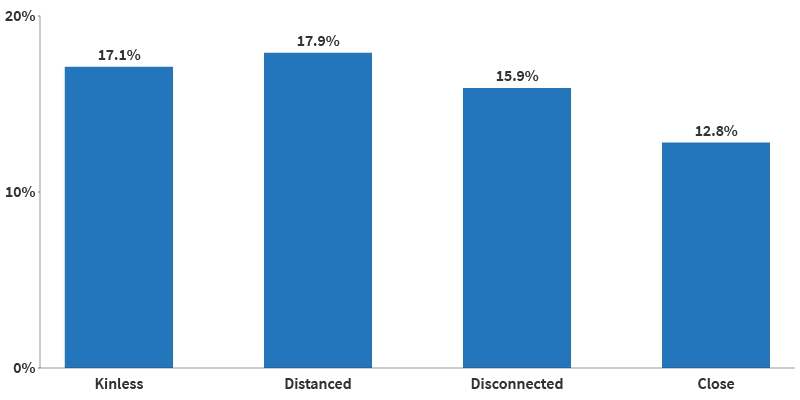
Source: Sarah E Patterson and Rachel Margolis, “Family Ties and Older Adult Well-Being: Incorporating Social Networks and Proximity,” The Journals of Gerontology: Series B, Volume 78, no. 12 (December 2023): 2080–89.
The findings suggest that the presence and strength of family ties matter for older adults’ mental health. “As families continue to evolve, researchers should strive to capture the size and shape of family networks, as well as the level of connection that older adults have with those kin,” the authors note.
In fact, social connections can also produce distress. Stephanie T. Child and Leora E. Lawton of UC Berkeley found that social companionship and emergency help mattered most to older adults, whereas having more people from whom they sought advice was related to more psychological distress.16 The findings suggest that mental well-being may be enhanced by enjoyable and helpful relationships, while those that are more demanding may detract from it. Data are from the UC Berkeley Social Networks Study (UCNets), which includes a locally representative sample from across the San Francisco Bay Area in California.
Companionship and emergency help mattered most to older adults.
In a similar study, the Berkeley authors found that those who were more dissatisfied with their social networks also experienced more loneliness and isolation.17 Interestingly, it wasn’t the number of connections but the closeness of the relationships—especially with family—that buffered loneliness. Further, having a romantic partner helped older adults feel less isolated.
As Child and Lawton write, “evaluations about one’s own social network, including whether someone feels satisfied in the number or quality of connections they have to call on for social engagement or support, may be a more meaningful precursor of loneliness.”
Similarly, social engagement may be connected to cognitive benefits. Using Michigan Cognitive Aging Project data, Abbey M. Hamlin at the University of Michigan and colleagues find important differences by race in both social engagement and its connection to cognition.18 Older white, non-Hispanic adults engaged in more social activities than their Black peers, and those activities were linked to better episodic memory—or the recall of information from the past—and thus better cognitive health. The findings suggest that social isolation is not only more prevalent among older non-Hispanic Black adults, but also that it may be taking a toll on their cognitive well-being.
Marriage Has Diverse Effects on Older Adults’ Health
Several recent studies build on the well-established link between marriage and better physical and psychological health in old age, particularly for men. They examine some of the ways marriage may benefit health as well as the connections between marriage and other forms of social interaction.
New research finds that marriage can help men be less socially isolated throughout their lives. Umberson of University of Texas at Austin, Zhiyong Lin of University of Texas at San Antonio, and Hyungmin Cha of USC show that men tend to be more isolated in adolescence and young adulthood, while women tend to experience isolation in later life.19 Their analysis of HRS data shows that levels of social isolation increase with age for both men and women.
But gender patterns differ by marital history (see Figure 3). Among older adults in stable marriages, women are less isolated than men until age 60, but by age 68, men are slightly less isolated than women. This gender gap shrinks at older ages for those who have experienced marital disruptions, possibly because chronic health issues contribute more to social isolation among women, the authors note.
Figure 3. Social Isolation Increases With Age, but Gender Patterns Differ by Marital History
Age Trajectories of Social Isolation Among Adults Ages 50 and Older, by Gender and Relationship History, 1998-2012
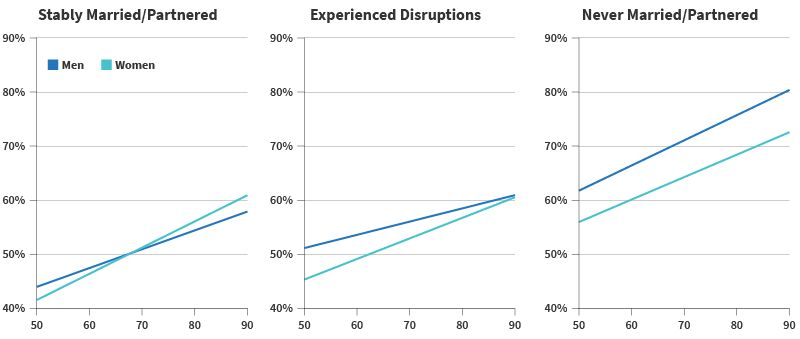
Source: Debra Umberson, Zhiyong Lin, and Hyungmin Cha, “Gender and Social Isolation Across the Life Course,” Journal of Health and Social Behavior 63, no. 3 (2022): 319-35.
There may be an unexpected physiological explanation for some of marriage’s health benefits. Drawing on lessons from primate research and using stool samples from a subset of participants in the long-running Wisconsin Longitudinal Study, researchers affiliated with the University of Wisconsin-Madison find that spouses in self-described close marriages tend to have more diverse and healthful gut microbiota compared with siblings, people without a partner, or married couples in less close relationships.20 Less diverse gut microbiota is related to obesity, cardiac disease, type 2 diabetes, and other inflammatory disorders, Kimberly Dill-McFarland and coauthors note.
Not all marriages are equal when it comes to social support and its potential health effects. Both men and women in same-sex marriages are more likely than those in different-sex marriages to offer concrete support to a spouse in distress, such as taking over chores or giving extra personal time, found Mieke Thomeer of the University of Alabama at Birmingham, Amanda Pollitt of Northern Arizona University, and Umberson.21 The team used a survey of 378 midlife couples ages 35 to 65.

Among older adults in stable marriages, men are less isolated than women.
Relationships can be a source of stress as well as support, and individuals in a marriage with a difficult or demanding partner experience a similar degree of loneliness as single people and more loneliness than other married people, another study finds.22 Shira Offer’s research at UC Berkeley draws on UCNets data to identify these differences and finds that the same is true for tough relationships with adult children.
Two other studies offer new insights into the mental health toll of the loss of a spouse due to death, separation, or divorce. People with less than a high school education face a higher risk of losing a spouse than people with more education, research using HRS data shows. But higher education levels do not lessen symptoms of depression when divorce, separation, or death does occur, find Claudia Recksiedler of the German Youth Institute and Robert S. Stawski of Oregon State University.23
People who lose a spouse often receive helpful support from social networks. Using NSHAP data, James Iveniuk of the Wellesley Institute and coauthors find that friends and family of older adults respond with social support after the death of a spouse, but less so when a close friend or other confidant dies.24
Good Neighbors (and Neighborhoods) Are Good for Well-Being
Multiple studies have shown that a neighborhood’s physical features—from broken sidewalks and high crime to plentiful parks and low air pollution—are related to older residents’ health and quality of life.25 Not surprisingly, the places older people call home also shape their social connections, thereby influencing both their physical and mental health.
Neighborhood social ties may promote sensory health, a study using NSHAP data shows. Older adults who have more social connections in their neighborhoods report better self-rated vision than those who have fewer connections, find Alyssa Goldman of Boston College and Jayant Pinto of the University of Chicago.26 More social ties may lead to more time spent engaging with people and places outside of the home, protecting visual abilities, the researchers suggest. Good vision is key to older adults’ ability to safely navigate their environment, they add.
For caregivers, social support can counteract the negative effects of living in less-connected neighborhoods. Researchers at the University of California, Davis and the University of Michigan show that neighborhoods with low social cohesion—lacking a sense of community and trust among neighbors—can take a toll on mental health in the absence of social support.27 This is particularly true for dementia caregivers, who face a high risk of depression related to the emotional and physical burden of their work. But dementia caregivers living in neighborhoods with low social cohesion had fewer symptoms of depression if they had family and friends to talk to and help with daily tasks, Oanh Meyer and team found.

Local opportunities for social connection may strengthen social ties.
Community-level interventions focused on increasing neighborhood connections—such as caregiver support groups in disadvantaged neighborhoods—could be important for maintaining caregiver health, the research team suggests.
The proximity of one’s close friends also makes a difference for mental health, reports Keunbok Lee of UCLA.28 Older adults with fewer confidants who live nearby show more severe depression symptoms when faced with traumatic events than those with more close friends in their neighborhood, according to Lee’s study of UCNets data.
When faced with traumatic events, older adults with fewer confidants living nearby showed more severe depression symptoms than those with more close friends in their neighborhood.
Local opportunities for social connection may strengthen social ties and help prevent suicide. A new study finds that suicide rates are much lower among working-age adults, including people ages 51 to 64, in counties with more places for people to connect, such as public libraries, community centers, religious groups, coffee shops, diners, and entertainment and sports venues.29 These findings held true even when the researchers accounted for differences in health care availability, age, education, race/ethnicity, and proximity to metropolitan areas.
Gathering places, part of the social infrastructure, may buffer suicide risk and improve mental health by boosting social connections, reducing social isolation, and facilitating social support, trust, and information and resource sharing, report Xue Zhang and Danielle Rhubart of Penn State University and Shannon Monnat of Syracuse University. Local governments should consider partnering “with market-based services and social service agencies to increase the availability, access, and use of spaces that promote social interaction,” they write. In addition to helping to lower suicide rates, building more robust social infrastructure may also support overall health, they suggest.
Living Alone Linked to Social Isolation and a Variety of Health Risks
Research has established that living alone at older ages raises the risk of poor health, early death, and dementia. New evidence demonstrates that living alone for extended periods increases the risk of dementia more strongly than previously thought.30 Every two years of living alone is linked to about a 10% increase in the risk of dementia, according to study authors Benjamin A. Shaw of the University of Illinois Chicago, Tse-Chuan Yang of the University of Albany, and Seulki Kim of the University of Nebraska.
Social isolation may explain this dynamic. Their analysis, based on HRS data that tracked more than 18,000 older Americans for 18 years (2000 to 2018), suggests that a lack of mental stimulation combined with limited day-to-day companionship may increase stress “that, over time, could accumulate and eventually lead to cognitive impairment.”
Even two years of living alone is linked to about a 10% increase in the risk of dementia.
Another recent study shows that the impact of social isolation extends to diet and nutrition. Analysis of data from an HRS nutrition survey shows that older adults—particularly men—living alone with no adult children or friends in their neighborhood had the lowest fruit and vegetable intake.31 Lack of motivation to cook and eat healthy may explain this pattern, according to Yeon Jin Choi, Jennifer A. Ailshire, and Eileen M. Crimmins of USC.
Because fruits and vegetables provide key nutrients for maintaining health and protecting against age-related diseases, the researchers recommend local agencies consider ways to improve social engagement among older adults who live alone to boost health outcomes. They also suggest providing help with grocery shopping (such as transportation) and meal preparation (including home-delivered meals).
Virtual Interaction Cannot Fully Replace the Health Benefits of Face-to-Face Contact
Phone calls and Zoom or FaceTime gatherings replaced in-person get-togethers for many people during the COVID-19 pandemic shutdowns, but a growing body of research suggests virtual interaction cannot fully replace face-to-face contact. Two recent studies, one led by Namkee Choi at the University of Texas at Austin and the other by Louise Hawkley at NORC at the University of Chicago, show that older adults who had less in-person time with family and friends and more phone calls during the first year of the pandemic were more likely to experience loneliness.32
Phone calls are an important source of social connection for older adults with impaired vision or hearing.
Older people with impaired hearing or vision may be an exception—phone and video chats appear to have protected them in 2020 from depressive symptoms, find Amanda Zhang and colleagues at the University of Chicago.33 One reason may be that phone calls are important for the mental health and mood of people with small social networks, replacing some of the day-to-day interactions that shrink with age and physical impairment, report Yijung K. Kim and Karen L. Fingerman of the University of Texas at Austin, based on another study.34
Older adults who had less in-person time with family and friends and more phone calls during the first year of the pandemic were more likely to experience loneliness.
At the root of these mixed findings on digital versus in-person interaction may be the immune system. A team of researchers from Colorado State University and UCLA show that face-to-face interaction protects health-promoting immune functions in ways that digital contact does not.35 They examined the gene activity that stimulates inflammation and inhibits antiviral responses in the blood of adult study participants during the COVID-19 social distancing period. Participants who had mainly online social contact had higher levels of such unhealthy gene activity than those who had more in-person social contact.
“Digitally mediated social relations do not appear to substantially offset the absence of in-person/offline social connection,” the research team concluded.
Policy Implications
As many as one in four older Americans are socially isolated and face an increased risk of poor health and early death. The research documented in this report underscores the links between strong social ties and longer, healthier lives. U.S. Surgeon General Vivek H. Murthy has called for making social connectedness a national priority, “the same way we have prioritized other critical public health issues such as tobacco, obesity, and substance use disorders.”36 His recent advisory, Our Epidemic of Loneliness and Isolation, identifies multiple actions based on growing research evidence, including:
- Strengthening social infrastructure: Social ties are not just built by person-to-person interactions, but by the physical elements (parks, libraries, sidewalks, and benches) and the programs and policies in place. Communities can design environments, establish and expand programs, and invest in institutions that bring people together.
- Enacting pro-connection public policies: National, state, local, and tribal governments can play a role in establishing policies for accessible public transportation, paid family leave, and other supports that can enable more connection among communities and families.
Social Isolation and Loneliness Among Older Adults: Opportunities for the Health Care System, a recent report from the National Academies of Sciences, Engineering, and Medicine, details ways health care organizations can address social isolation among older people by better educating their staff to intervene and aligning with other community agencies. Specific recommendations include:
- Partnering directly with ride-sharing programs to help older adults’ get to medical appointments and community events.
- Working with community organizations to integrate social activities and in-person interaction into hospital discharge planning, care coordination, and transitional care planning.
“Our relationships are a source of healing and well-being hiding in plain sight,” Murthy said, “one that can help us live healthier, more fulfilled, and more productive lives.”37

Accessible public transportation can help improve older adults’ health by connecting them to both medial care and social activities.
References
- Kelly E. Rentscher et al., “Social Relationships and Epigenetic Aging in Older Adulthood: Results From the Health and Retirement Study,” Brain, Behavior, and Immunity 114, (2023): 349-59.
- Linda Waite and Yiang Li, “Bringing the Social World Into Our Understanding of Health,” paper presented at the annual meeting of the Population Association of America, Columbus, April 2024.
- Michaela G. Cuneo et al., “Positive Psychosocial Factors and Oxytocin in the Ovarian Tumor Microenvironment,” Psychosomatic Medicine 83, no. 5 (2021): 417-22.
- Dannielle E. Kelley, et al., “Dyadic Associations Between Perceived Social Support and Cancer Patient and Caregiver Health: An Actor-Partner Interdependence Modeling Approach,” Psycho-oncology 28, no. 7 (2019): 1453-60.
- Won-Tak Joo, “Educational Gradient in Social Network Changes at Disease Diagnosis,” Social Science & Medicine 317 (2023): 115626.
- Karen L. Fingerman, et al., “Functional Limitations, Social Integration, and Daily Activities in Late Life,” The Journals of Gerontology: Series B, Psychological Sciences and Social Sciences 76, no. 10 (2021): 1937-47.
- Sophie Mitra, Debra L. Brucker, and Katie M Jajtner, “Wellbeing at Older Ages: Towards an Inclusive and Multidimensional Measure,” Disability and Health Journal 13, no. 4 (2020): 100926.
- Dan Zhang et al. “What Could Interfere with a Good Night’s Sleep? The Risks of Social Isolation, Poor Physical and Psychological Health Among Older Adults in China,” Research on Aging 44, nos. 7-8 (2022): 519-30.
- Debra Umberson and Rachel Donnelly, “Social Isolation: An Unequally Distributed Health Hazard,” Annual Review of Sociology 49, no. 1 (2023): 379-99.
- Thomas K. M. Cudjoe et al., “The Epidemiology of Social Isolation: National Health and Aging Trends Study,” The Journals of Gerontology: Series B, Psychological Sciences and Social Sciences 75, no. 1 (2020): 107-13.
- Kaulie Watson, “Social Isolation Can Begin as Early as Adolescence, Research Shows,” The University of Texas at Austin College of Liberal Arts, July 20, 2023.
- Jordan Weiss, Leora E. Lawton, and Claude S. Fischer, “Life Course Transitions and Changes in Network Ties Among Younger and Older Adults,” Advances in Life Course Research 52 (2022): 100478.
- James Iveniuk, “Social Networks, Role-Relationships, and Personality in Older Adulthood,” The Journals of Gerontology: Series B, Psychological Sciences and Social Sciences, 74, no. 5, July 2019, 815–26.
- Sarah E. Patterson and Rachel Margolis, “Family Ties and Older Adult Well-Being: Incorporating Social Networks and Proximity,” The Journals of Gerontology: Series B Psychological Sciences and Social Sciences, 78, no. 12 (2023): 2080-9.
- Jon Meerdink, “New Paper Explores the Impact of Family Ties on Older Adults,” University of Michigan Institute for Social Research, November 15, 2023.
- Stephanie T. Child and Leora E. Lawton, “Personal Networks and Associations With Psychological Distress Among Young and Older Adults,” Social Science & Medicine 246 (2020): 112714.
- Stephanie T. Child and Leora Lawton, “Loneliness and Social Isolation Among Young and Late Middle-Age Adults: Associations With Personal Networks and Social Participation,” Aging & Mental Health 23, no. 2 (2019): 196-204.
- Abbey M. Hamlin et al., “Social Engagement and Its Links to Cognition Differ Across Non-Hispanic Black and White Older Adults,” Neuropsychology 36, no. 7 (2022): 640-50.
- Debra Umberson, Zhiyong Lin, and Hyungmin Cha, “Gender and Social Isolation Across the Life Course,” Journal of Health and Social behavior 63, no. 3 (2022): 319-35.
- Kimberly A. Dill-McFarland et al., “Close Social Relationships Correlate With Human Gut Microbiota Composition,” Scientific Reports 9, no. 1 (2019): 703.
- Mieke Beth Thomeer, Amanda Pollitt, and Debra Umberson, “Support in Response to a Spouse’s Distress: Comparing Women and Men in Same-Sex and Different-Sex Marriages,” Journal of Social and Personal Relationships 38, no. 5 (2021): 1513-34.
- Shira Offer, “They Drive Me Crazy: Difficult Social Ties and Subjective Well-Being,” Journal of Health and Social Behavior 61, no. 4 (2020): 418-36.
- Claudia Recksiedler and Robert S. Stawski, “Marital Transitions and Depressive Symptoms Among Older Adults: Examining Educational Differences,” Gerontology 65, no. 4 (2019): 407-18.
- James Iveniuk, Peter Donnelly, and Louise Hawkley, “The Death of Confidants and Changes in Older Adults’ Social Lives,” Research on Aging 42, nos. 7-8 (2020): 236-46.
- Mark Mather and Paola Scommegna, “How Neighborhoods Affect the Health and Well-Being of Older Americans,” Today’s Research on Aging, no. 35 (2017).
- Alyssa Goldman and Jayant Pinto, “Sensory Health Among Older Adults in the United States: A Neighborhood Context Approach,” The Journals of Gerontology: Series B; Psychological Sciences and Social Sciences, 79, no. 5, (May).
- Oanh L. Meyer et al., “Neighborhood Characteristics and Caregiver Depressive Symptoms in the National Study of Caregiving,” Journal of Aging and Health 34, no. 6-8 (2022): 1005-15.
- Keunbok Lee, “Different Discussion Partners and Their Effect on Depression Among Older Adults,” Social Sciences 10, no. 6 (2021): 215.
- Xue Zhang, Danielle Rhubart, and Shannon Monnat, “Social Infrastructure Availability and Suicide Rates Among Working-Age Adults in the United States,” Socius 10 (2024).
- Benjamin A Shaw, Tse-Chuan Yang, and Seulki Kim, “Living Alone During Old Age and the Risk of Dementia: Assessing the Cumulative Risk of Living Alone,” The Journals of Gerontology: Series B, Psychological Sciences and Social Sciences 78, no. 2 (2023): 293-301.
- Yeon Jin Choi, Jennifer A. Ailshire, and Eileen M. Crimmins, “Living Alone, Social Networks in Neighbourhoods, and Daily Fruit and Vegetable Consumption Among Middle-Aged and Older Adults in the USA,” Public Health Nutrition 23,18 (2020): 3315-23.
- Namkee G. Choi et al., “COVID-19 and Loneliness Among Older Adults: Associations With Mode of Family/Friend Contacts and Social Participation,” Clinical Gerontologist 45, no. 2 (2022): 390-402 and Louise C. Hawkley et al., “Can Remote Social Contact Replace In-Person Contact to Protect Mental Health Among Older Adults?” Journal of the American Geriatrics Society 69, no. 11 (2021): 3063-5.
- Amanda Zhang et al., “Can Digital Communication Protect Against Depression for Older Adults With Hearing and Vision Impairment During COVID-19?” The Journals of Gerontology: Series B, Psychological Sciences and Social Sciences 78, no. 4 (2023): 629-38.
- Yijung K. Kim, and Karen L. Fingerman, “Daily Social Media Use, Social Ties, and Emotional Well-Being in Later Life,” Journal of Social and Personal Relationships 39, no. 6 (2022): 1794-1813.
- Jeffrey G. Snodgrass et al. “Social Connection and Gene Regulation During the COVID-19 Pandemic: Divergent Patterns for Online and In-Person Interaction,” Psychoneuroendocrinology 144 (2022): 105885.
- U.S. Department of Health and Human Services, “New Surgeon General Advisory Raises Alarm About the Devastating Impact of the Epidemic of Loneliness and Isolation in the United States,” May 3, 2023.
- U.S. Department of Health and Human Services, “New Surgeon General Advisory Raises Alarm About the Devastating Impact of the Epidemic of Loneliness and Isolation in the United States.”