Heidi Worley
Former Program Director

November 6, 2013
Former Program Director
Technical Director, Demographic Research
Twenty years after its civil war ended in 1992, Mozambique has made significant progress. Economic growth has remained steady for over a decade. Malaria prevalence in children has declined and households are more protected by insecticide-treated nets or indoor spraying. More than one-half of all childbirths occur in health facilities. And early childhood mortality is declining dramatically, with half as many deaths among children under 5, compared to 14 years ago (see figure).
Early Childhood Mortality Is on the Decline in Mozambique.
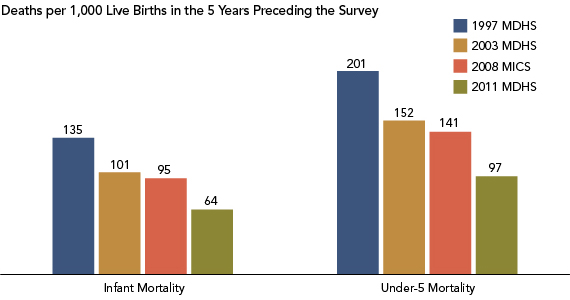
Note: MDHS refers to the Mozambique Demographic and Health Survey; MICS refers to the Multiple Indicator Cluster Survey.
Sources: Instituto Nacional de Estatística, Ministério da Saúde, Maputo, Moçambique, and ICF International, Mozambique Demographic and Health Survey 2011 (Calverton, MD: ICF International, 2013); United Nations Children’s Fund (UNICEF) and Instituto Nacional de Estatística, Maputo, Moçambique, Mozambique Multiple Indicator Cluster Survey 2008-2009 (New York: United Nations Children’s Fund (UNICEF), 2009); Instituto Nacional de Estatistica, Ministerio da Saude, Maputo, Moçambique and ORC Macro, Mozambique Demographic and Health Survey 2003 (Calverton, MD: ORC Macro, 2005); andManuel da Costa Gaspar et al., Instituto Nacional de Estatística, Maputo, Moçambique, and Macro International, Mozambique Demographic and Health Survey 1997 (Calverton, MD: Macro International Inc., 1998).
The country recently released a final report from its 2011 Mozambique Demographic and Health Survey (MDHS), lending evidence to this progress but highlighting areas where gaps remain. Fertility rates are still high (average of 5.9 children per woman), and in fact have risen slightly since the last MDHS in 2003 (5.5 children per woman). Fertility is lower for better-educated and wealthier women, and those living in urban areas.1
Knowledge of modern contraceptive methods is common, yet contraceptive use remains low, and unmet need for family planning is generally high across women of all backgrounds, with one in four married women expressing an unmet need for family planning (meaning they do not want to become pregnant for two years or more but are not using a modern contraceptive method). Mozambique continues to have a high level of early childbearing, affecting over one-third of women ages 15 to 19, although as education levels increase, teen pregnancy is less common. This group has the highest unmet need for family planning: While one quarter use modern contraception, over half still express the desire to limit births. And maternal mortality remains high at 408 deaths per 100,000 live births.2
To help inform decisionmakers about these gaps, PRB was asked, through its IDEA project, to develop a policy communications strategy to disseminate the 2011 MDHS to refocus attention on population, family planning, and health policies and programs. IDEA (Informing Decisionmakers to Act) provides information about family planning and reproductive health to policy audiences around the world. IDEA received support from USAID/Mozambique to partner with the Mozambican Instituto Nacional de Estatistics (INE) that conducted the 2011 survey.
IDEA staff collaborated with the staff from INE and the Mozambique Ministry of Health to develop a set of publications in Portuguese and English for provincial policymakers and other decisionmakers, educators, and journalists. (Several of the publications, in Portuguese, are online and linked below.) These included:
On May 2, 2013, the national MDHS launched its findings. Following the launch, the IDEA products were disseminated during provincial-level meetings, sectoral meetings, and one-day media training workshops in 10 provinces and Maputo. At these meetings, INE used the products to raise awareness of areas requiring further attention and investment from local leaders. Toshiko Kaneda, the project leader and a senior research associate at PRB, said of PRB’s role in this process, “A huge amount of effort goes into collecting data, but they (INE) don’t feel like the data get enough use. That’s why a project like ours that tries to promote the use of the data by making the results accessible to policymakers, other decisionmakers, and nontechnical audiences is so important. “
Feedback from these meetings was positive. At least 30 percent of participants gave comments that reflected their intention to further use the data in their work: Requests came for access to more data, district-level disaggregation, and future coverage or content improvements. Kaneda reported, “INE was excited about the excellent feedback they were getting from all the print publications. They said they will be very beneficial as they promote the use of the MDHS results in policy planning, which they are trying to improve at the provincial-level.” Project consultant Marjorie Macieira noted that “INE expressed how helpful to them it was to have PRB participate in the selection and definition of key indicators, and with the actual design and development of the thematic brochures.”
Data from the MDHS, made accessible by PRB, can help decisionmakers and program planners to address health problems. Mozambique is located in southern Africa, the region with the highest prevalence of HIV in the world. More than 10 percent of adults ages 15 to 49 in Mozambique are living with HIV.3 According to the MDHS, neither women nor men have a comprehensive knowledge of HIV/AIDS and its prevention. Three-quarters of men know ways to prevent HIV, such as condom use and limiting sex to one uninfected partner, but only half of women share this knowledge. Risky sexual behavior is common (30 percent of men had two or more sexual partners in the last year before the survey) but few have undergone testing. Young people are a priority group for HIV-prevention activities throughout the region, especially given that early initiation of sexual activity is common: More than three-quarters of women ages 20 to 24 were sexually active before age 18, compared to two-thirds of men.4 The MDHS data can help health educators craft evidence-based programs to address these pressing problems, such as delaying the age of sexual activity initiation as a strategy to reduce the risk of HIV infection among youth.
Journalists, especially those who undergo media training, can use the MDHS data to make the numbers come alive in their stories. Macieira shared, “Another challenge was getting the media’s attention focused on disseminating the 2011 MDHS findings because of the generally less appealing interest of ‘statistical information.’ The media is more likely to cover breaking political developments and will need additional training to get them educated on maximizing use of the MDHS findings in their daily news coverage,” a plan, she noted, that INE already has in process.

July 2, 2002
Senior Fellow, Futures Group International
Despite the fact that sub-Saharan Africa contains only about 11 percent of the Earth’s population, the region is the world’s epicenter of HIV/AIDS. The numbers are daunting. Adult HIV prevalence is 1.2 percent worldwide (0.6 percent in North America), but it is 9.0 percent in sub-Saharan Africa. UNAIDS estimates that at the end of 2001, there were 40 million people living with HIV/AIDS, 28.5 million of them from sub-Saharan African. Five million adults and children became newly infected with HIV in 2001, 3.5 million of them from sub-Saharan Africa. Three million people died from AIDS-related causes in 2001, and 2.2 million of these deaths were among sub-Saharan Africans.2
AIDS is now the leading cause of death in sub-Saharan Africa. (Worldwide, AIDS is the fourth leading cause of death.) Life expectancy at birth has plummeted in many African countries, wiping out the gains made since independence. The combination of high birth rates and high AIDS mortality among adults, including many parents, has meant that more than 90 percent of children who have been orphaned as a consequence of the HIV/AIDS epidemic are in this region.2
These statistics disguise an important part of the story, however. Most of the worst affected countries form an “AIDS belt” in eastern and southern Africa. This belt consists of about 16 countries3 and stretches from Djibouti and Ethiopia down the east side of the continent through South Africa. These countries constitute only a little more than 4 percent of the world’s population but account for more than 50 percent of HIV infections worldwide.
According to UNAIDS, all the worst affected countries (with prevalence rates over 20 percent) are contiguous to one another in the lower part of the continent. These include South Africa, Lesotho, Swaziland, Botswana, Namibia, Zambia, and Zimbabwe. Botswana, Lesotho, Swaziland, and Zimbabwe have prevalence rates above 30 percent.4
Further north in the AIDS belt, Mozambique, Malawi, Burundi, Rwanda, Kenya, Tanzania, and Ethiopia all have adult prevalence rates in the 6-15 percent range. Adult prevalence in Uganda is estimated to be around 5 percent. Uganda is the one country in the region that has probably achieved a longstanding decline in HIV prevalence. Prevalence in Uganda may have peaked in the 12-13 percent range in the early 1990s before the onset of this decline.
Elsewhere, Somalia, Eritrea, Djibouti, and Sudan have little or no data, and Madagascar remains an interesting case. Despite tourism, an active commercial sex trade, and high rates of other sexually transmitted infections (STIs), and despite being separated from the African mainland by only 60 kms of water, adult HIV prevalence remains below 1 percent.5
Though having overall adult prevalence rates lower than in the eastern and southern parts of the continent, the middle part of Africa6 is undergoing a serious and generalized7 HIV/AIDS epidemic. Among the countries in the region, the Democratic Republic of Congo, Chad, and Equatorial Guinea show adult HIV prevalence rates under 5 percent. Angola has been war-torn and chaotic for so long that it is difficult to know exactly what is transpiring with the epidemic there. However, UNAIDS places the adult prevalence rate at 5.5 percent. Elsewhere in the region, UNAIDS reports prevalence rates of 7.2 percent in the Congo, 11.8 percent in Cameroon, and 12.9 percent in the Central African Republic.8 Many of the worst affected countries in middle Africa have the highest rates of other STIs on the continent.
Among the 15 countries of West Africa,9 only a few countries have prevalence rates over 5 percent. These include Burkina Faso (6.5 percent), Côte d’Ivoire (9.7 percent), Nigeria (5.8 percent), and Togo (6.0 percent). With an estimated population of 127 million, Nigeria is the demographic giant of sub-Saharan Africa. After South Africa, Nigeria has more people living with HIV/AIDS (3.5 million in 2001) than any other place on the continent. Côte d’Ivoire receives a large number of male migrants from neighboring countries who are temporary workers. Along with a vibrant commercial sex industry, especially in the capital city of Abidjan, this helps explain why Côte d’Ivoire has emerged as the epicenter of the epidemic in West Africa.
Table 1
Estimated Number of People in the African “AIDS Belt” Living with HIV/AIDS, end of 2001
| Total Adults and Children | Total Women (15-49) | Adults (15-49) rate (%) | |
|---|---|---|---|
| Global Total | 40 million | 18.5 million | 1.2 |
| Sub-Saharan Africa | 28.5 million | 15 million | 9.0 |
| Djibouti | – | – | – |
| Ethiopia | 2.1 million | 1.1 million | 6.4 |
| Uganda | 600,000 | 280,000 | 5.0 |
| Kenya | 2.5 million | 1.4 million | 15.0 |
| Tanzania | 1.5 million | 750,000 | 7.8 |
| Rwanda | 500,000 | 250,000 | 8.9 |
| Burundi | 390,000 | 190,000 | 8.3 |
| Mozambique | 1.1 million | 630,000 | 13.0 |
| Malawi | 850,000 | 440,000 | 15.0 |
| Zambia | 1.2 million | 590,000 | 21.5 |
| Zimbabwe | 2.3 million | 1.2 million | 33.7 |
| Namibia | 230,000 | 110,000 | 22.5 |
| Botswana | 330,000 | 170,000 | 38.8 |
| Swaziland | 170,000 | 89,000 | 33.4 |
| Lesotho | 360,000 | 180,000 | 31.0 |
| South Africa | 5.0 million | 2.7 million | 20.1 |
Source: UNAIDS, Report on the Global HIV/AIDS Epidemic: July 2002.
Why have rates in West Africa not soared to the levels found in the AIDS belt countries of eastern and southern Africa? If the African epidemic has its roots in the Great Lakes region, the epicenter could well have moved westward into middle and western Africa. Instead, it moved primarily southward. The question is an intriguing one and no consensus has emerged in response. Cultural and social norms may have played a role.10 For example, in countries with conservative Islamic traditions and a large proportion of Muslims in the population, sexual networking may be more circumscribed than in other countries.
Demographers John and Pat Caldwell suggest at least two additional factors. They point out that the presence of other STIs is probably the single most important factor contributing to the rapid spread of HIV. However, it is not all STIs, but especially those that cause genital ulcers that serve as an effective conduit of HIV. In West Africa, gonorrhea is the most common STI, but this is a non-ulcerative STI and an ineffective transmitter of HIV. By contrast, syphilis and chancroid are the dominant STIs in eastern and southern Africa. Both are ulcerative STIs that greatly increase the probability of HIV transmission.
Also, in most societies in West Africa, male circumcision is almost always practiced, while it is uncommon in a very large swathe of the AIDS-belt countries.11 Several studies conducted over the last decade and a half point to an association between male circumcision in some areas of sub-Saharan Africa and a reduced risk of HIV infection. However, it is still not clear whether circumcision’s apparent protective effect is due to culturally or religiously dictated behaviors — such as limiting the number of sex partners — or what the foreskin’s biological role is in male infection with HIV and other STIs.
Is the epidemic still worsening or is the situation improving? Uganda is still the only country in the region that has achieved a sustained decline in HIV prevalence. In some places — parts of Zambia, for example — prevalence appears to be dropping among the younger age groups, a possible prelude to an overall prevalence decline.
UNAIDS indicates that in 2000 the number of annual new infections went down for the first time relative to the previous year.12 While this is an encouraging trend, a drop in the annual number of new infections over a short period does not mean very much by itself. Some eventual downturn in incidence (annual new infections) would eventually occur even in the absence of any successful prevention efforts. The high levels of incidence that drove expansion of the epidemic during the 1990s could not be sustained indefinitely. This happens, in part, because prevalence levels become so high in certain high-risk groups that there is little room for expansion. A drop in incidence over a number of years is needed before it signifies a change in the overall course of the epidemic. Also, a rise in a few key but large countries — Congo and Nigeria, for example — could see incidence climbing again.
The best assessment is that, while there are some hopeful signs, overall the epidemic continues to rage throughout the Africa region. Even if prevention efforts become radically more successful in the near future than they have been, the impacts of the HIV/AIDS epidemic are going to echo for generations. If prevention, treatment, and care programs evolve at a more modest pace, it is certain that HIV/AIDS will have a profound impact on African development well into the 21st century.

April 1, 2000
(April 2000) The floods in southern Africa have turned world attention and resources to Mozambique. International donors have flown in emergency shipments of food, medical supplies, and search and rescue personnel to lessen human suffering and minimize the death toll — 500 confirmed and hundreds more expected.
A far deadlier but less obvious problem besetting the southeastern African country is maternal mortality. Maternal mortality, like the deaths from the floods, is difficult to measure; yet unlike a sudden natural disaster, the problem doesn’t make international news.
Mozambique’s ratio of maternal deaths to 100,000 live births — 1,500 — is among the world’s highest. With the country’s population of 19.6 million, the ratio translates into about 9,800 maternal deaths per year; roughly one in seven women die from pregnancy or childbirth complications. Often, the women who die leave behind other children, whose care may be jeopardized. In nearly every case, the deaths of women rob their families and societies of social support and productive workers.
Why is the toll so high? In fact, it could be higher. It’s difficult to measure maternal mortality because it requires accurate information about deaths of women ages 15 to 49. Few less-developed countries register births and deaths; fewer still record cause of death, which even in more-developed countries may elude health care workers if the women have tried to conceal or abort their pregnancies.
That is why the World Health Organization and UNICEF estimate maternal mortality rates and ratios for less-developed countries including Mozambique based on birth rates and the proportion of births that are assisted by a trained person. In the case of Mozambique, specialists use mathematical models to predict the proportion of all deaths of women of reproductive age that are maternal, and then apply this proportion to UN projections of adult female deaths.
There are three main reasons for Mozambique’s high maternal mortality:
These problems also help explain the country’s high infant mortality rate.
As of March 3, USAID’s total contribution to flood relief efforts amounted to $12.7 million. The agency’s fiscal year 2000 budget request for population and health programs in Mozambique totaled $14.5 million.
For More Information
Mozambique
Population: 19.6 million
GNP per capita, 1997: US$140
Total Fertility Rate: 5.6
Maternal Mortality Rate: 1,500 deaths per 100,000 live births
Infant Mortality Rate: 134 deaths per 1,000 live births
Source: PRB’s World Population Data Sheet, 1997 and 1999.
