Quick Links

Aging and Health in China: What Can We Learn From the World’s Largest Population of Older People?
No other country in the world is experiencing population aging on the same scale as China.
The United Nations projects that there will be 366 million older Chinese adults by 2050, which is substantially larger than the current total U.S. population (331 million).1By that time, China’s share of adults ages 65 and older wills have risen from just 12% to a projected 26%. This rapid population aging—driven by recent declines in fertility and mortality—raises concerns about the health and well-being of older Chinese adults and will create considerable challenges for the health care system.
While life expectancy in China is increasing, older adults may spend more of their advanced years in poor health and with disabilities. Families have been the primary source of care for older adults, but the country’s rapid economic development and urbanization have separated millions of older adults from their children, contributing to an increasing demand for community-based health care.
These demographic and socioeconomic changes raise important questions for researchers and policymakers. How are older Chinese adults faring relative to their parents’ and grandparents’ generations? How is rapid urbanization affecting health and the availability of potential caregivers among older adults? How are older women faring relative to men, and which factors contribute to the gender gap in health? More broadly, what are the key factors associated with healthy aging in China, and what can policymakers do to improve health and reduce health disparities in the context of the country’s rapid socioeconomic development?
This issue of PRB’s Today’s Research on Aging (Issue 39) summarizes recent research on aging and health in China from U.S. National Institute of Aging-sponsored investigators and surveys, especially the China Health and Retirement Longitudinal Study (CHARLS) and Chinese Longitudinal Healthy Longevity Study (CLHLS). Results from these studies can shed light on the key determinants of healthy aging and help identify policies to address the challenges posed by rapid population aging in China.2The findings can also offer insights to policymakers in other countries with rapidly growing older populations.
Life Expectancy Is Increasing but China’s Aging Population Faces Health Challenges
China’s life expectancy has increased steadily during the past half century. In 1960, average life expectancy at birth in China was around 44 years. By 2017, it had increased to 76 years.3
Physical and cognitive health among older adults—especially women—is also improving with rising educational attainment and better medical care.4
Yi Zeng and colleagues find evidence of morbidity compression among China’s older adults—a reduction in the proportion of life spent with disability. Among adults ages 80 and older, mortality and self- reported disability rates have fallen relative to cohorts born 10 years earlier, according to their analysis of CLHLS data.5A recent study of adults ages 50 and older, based on CHARLS data, shows that at age 50, men can expect to live 24 years without activity limitations (26 years for women).6
These life expectancy gains and reductions in disability, however, are linked to rapid economic development in urban areas. Older adults in rural areas have not fared as well, leading to growing rural-urban disparities in health.7
Rising obesity rates and high smoking prevalence (among men) also present major health challenges for China’s aging population. In 2011, 28% of men and 38% of women ages 45 and older were overweight, putting them at higher risk of heart disorders, hypertension, diabetes, and stroke.8 Over half of men ages 45 and older (53%) smoked in 2011, compared with 5% of women in that age group.9 High levels of pollution—especially in urban areas—pose additional health risks.
“Public health campaigns and incentives are urgently needed on all these fronts so that the predictable long-term consequences of these behaviors on older age disease are not realized,” report researchers James Smith and his colleagues.9
Supportive Policies Can Address the Caregiving Gap for Older Adults
Families have traditionally been the major source of financial and caregiving support for older adults in China, and most older adults have children living with them or nearby who can provide caregiving assistance. CHARLS data show that about 41% of older adults live with an adult child, and another 34% have an adult child living nearby.11
However, China’s relatively low fertility rate will reduce the availability of family caregivers in the future.12 Between 1980 and 2015, China applied a family planning policy limiting most families to only one child to control the country’s rapid growth. Adults ages 65 and older have five to six surviving children, on average, while younger cohorts born in the late 1950s and 1960s have fewer than two adult children on average.13 China’s total fertility rate (TFR), or average number of births per woman, is around 1.6. By comparison, the TFR in Asia as a whole (excluding China) is around 2.3, and the TFR in the United States is around 1.7.14
A growing number of young adults in China are also moving from rural to urban areas for employment opportunities. The share of the population living in urban areas increased from 19% in 1980 to 60% in 2019.15 This trend has left many older adults geographically separated from their adult children.16
Home- and community-based services could help fill the caregiving gap by providing older adults with medical, rehabilitation, and other healthcare services. These kinds of paid services are increasing but are not widely available, even in cities.17
As the demand for home-based care increases, the cost of providing that care will also increase with the rising number of disabled older adults. These costs include paid medical and nursing services, as well as opportunity costs for unpaid family members or friends who are providing care. Using CLHLS data, Zeng and colleagues find that older Chinese women are more likely than their male counterparts to become disabled. Yet expenditures on home-based care are lower for older women than men—an issue that needs more attention from policymakers, according to the study researchers.18
Chinese policymakers can promote healthy aging among older adults by implementing policies that address rural-urban disparities in health. Smith and colleagues argue that policies to help keep families together by allowing older adults to migrate to cities with their children could help reduce the caregiving gap in future years.19 Policymakers can also address older adults’ needs by expanding access to home- and community-based services, which older adults prefer over institutional (nursing home) care.20
Finally, the government could improve health and longevity by expanding access to health insurance coverage. By 2011, about 93% of Chinese adults ages 45 and older had health insurance. However, middle-aged and older adults with lower incomes were less likely to be insured—especially those with less education, divorced/widowed women, and those living in rural areas.21
Older Adults Report Worse Health in Poor, Rural Areas
Older adults in rural China face additional health challenges. Self-reported health status varies widely across different areas of the country, with people from poorer rural counties reporting the worst health status. In the poorer rural counties, half of adults ages 45 and older reported being in poor health in 2011-2012, compared with 9% in better-off urban counties (see figure).22
Poor self-reported health in rural areas may reflect a lack of public health investments relative to better-off urban counties. Smith and colleagues find that living in areas in China without a strong public health infrastructure is associated with worse health in old age. In particular, using surface water instead of tap or underground water and using a toileting system without water may negatively affect health, including general health status and activities of daily living such as dressing, bathing, eating, and getting into or out of bed.23
FIGURE 1: Older Chinese Living in Poorest Rural Counties More Likely to Report Poor Health
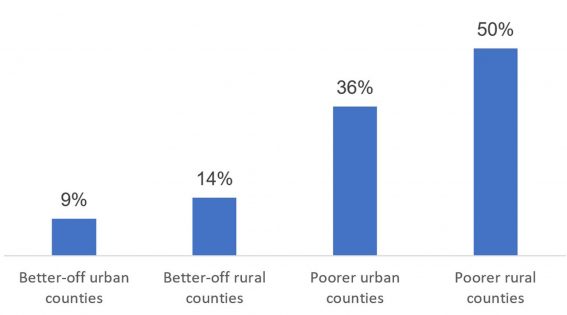
Self-Reported Health Status of Chinese Adults Ages 45 and Older, 2011-2012
Source: James P. Smith, Meng Tian, and Yaohui Zhao, “Community Effects on Elderly Health: Evidence from CHARLS National Baseline,” Journal of the Economics of Ageing 1-2 (2013): 50-59.
Health Behaviors and Pollution Pose Health Risks in Urban Areas
China’s rapid economic development has contributed to longer life expectancy, but it has also brought challenges related to lifestyle changes and pollution, particularly in urban areas.
Biological risk—measured biomarkers that reflect cardiovascular, metabolic, and inflammatory processes—is higher among older adults living in urban areas. This urban-rural gap in biological risk is largely explained by lifestyle factors such as lower levels of physical activity, according to a recent analysis of CHARLS data by Yuan Zhang and Eileen Crimmins.24 Another study of Chinese adults ages 65 and older, based on CHARLS data, showed that living in urban areas later in life is associated with better initial cognitive status but a faster rate of cognitive decline.25 The researchers argue that faster cognitive decline in cities may be linked to higher levels of population density and “constricted life space,” high housing costs, and the high cost of food and health services, among other factors.
China has also become one of the most polluted regions in the world, posing additional health risks for older adults—especially those living in cities. Long-term exposure to fine particulate matter in China is linked to greater risk of mortality in old age, while proximity to green space is associated with longer life expectancy.24 Older adults living in rural and southern areas are more sensitive to pollution than those residing in urban areas and in northern China, where pollution levels are higher. Higher sensitivity to pollutants in rural areas may be linked to time spent outdoors, health care access, baseline health status, or differences in the type of particulate matter present in rural and urban areas.26
Wide Gender Gaps in Health Persist
Older Chinese women fare worse than men across a wide range of health measures. In 2011, women ages 45 and older were more likely than men to report being in poor or very poor health; experience depression, body pain, and hypertension; and have difficulties with activities of daily living (see table).
TABLE: Older Chinese Women Experience Poor Health Relative to Men Health Differences Among Chinese Men and Women Ages 45 and Older
| Women (%) | Men (%) | |
| Poor or very poor health | 27.5 | 22.4 |
| High depressive symptoms | 40.7 | 28.1 |
| ADL/IADL difficulty | 29.6 | 21.8 |
| Body pain | 36.6 | 24.9 |
| Total hypertension | 43.9 | 40.3 |
| Undiagnosed hypertension | 39.6 | 42.8 |
| Get treatment if hypertensive | 48.8 | 44.6 |
Note: ADL means activities of daily living, such as dressing, bathing, eating, and getting into or out of bed. IADL means instrumental activities of daily living, such as shopping, cooking meals, managing money, and making phone calls.
Source: James P. Smith, John Strauss, and Yaohui Zhao, “Healthy Aging in China,” Journal of the Economics of Ageing 4, no. 2, (2014): 37-43.
Persistent gender gaps in education and literacy are partly to blame for older Chinese women’s poor health relative to men. Among adults ages 45 and older, about 40% of women were illiterate in 2011-2012, compared with 13% of men. Yet differences across age groups show the rapid progress women have made in recent years: The share of women ages 75 and older who were illiterate, at 80%, was 58 percentage points higher than the illiteracy rate among women ages 45 to 55 (22%).27
Researchers have also identified wide gaps in the cognitive abilities of older men and women. Gender differences in education largely explain this gap, especially among those in the oldest age groups and poorer communities. These gender differences in cognitive ability are decreasing as educational attainment increases among Chinese women in younger cohorts.29
Women’s childbearing patterns help explain the gender gap in health at older ages. Prior to the implementation of China’s one-child policy in 1980, women commonly had many children and started bearing them at a young age, which can negatively affect women’s health. Researchers have found that these effects can carry over into old age: Chinese women with four or more children are more likely to experience disabilities (impairment of activities of daily living, such as trouble dressing, bathing, eating, and getting into or out of bed) and poor self-rated health than women with one to three children.30
Conditions in childhood may also help explain gender gaps in health later in life. Using CLHLS data, Ke Shen and Yi Zeng find that favorable childhood conditions—based on birthplace, father’s socioeconomic status, and access to medical care in childhood—are linked to longer life expectancy through better socioeconomic status in adulthood.
“Public policies that target childhood well-being could effectively improve socioeconomic achievements in adulthood and, in turn, promote good health at senior ages,” argue researchers Shen and Zeng.31
However, this positive association is partially offset by “mortality selection.” The mortality selection hypothesis argues that unfavorable childhood circumstances result in high mortality rates among the most vulnerable people within a population and longer longevity for those who reach adulthood. This selection effect is larger for women than for men, possibly because surviving females tend to be healthier in countries with a strong son preference.32
“A girl might have worse nutrition and receive less care than a boy might. Such gender discrimination increases the mortality of vulnerable female infants, thus the surviving women are more selectively robust and have a higher chance of living into advanced ages,” according to the researchers.
Conclusion
China’s rapid economic development and urbanization may be a double-edged sword in their potential effects on the health and well-being of older adults. On the one hand, rapid economic growth has contributed to rising life expectancy and lower levels of disability. Rising educational attainment, especially among women, should lead to further improvements in health and reductions in health disparities among older adults. China’s health care system has also improved as the government has expanded access to public health services in both urban and rural areas.
On the other hand, rapid urbanization is separating millions of older adults from their adult children. Rising obesity rates, high smoking prevalence, and high levels of pollution also raise serious concerns about the health of China’s older adults in the coming decades.
These health challenges will be exacerbated by rapid demographic change. China has the world’s largest population of older adults and is experiencing population aging on an unprecedented—and unstoppable—scale.
China’s challenges will be shared by leaders in many other developing countries that have experienced rapid declines in fertility and mortality in recent decades. Studying the factors associated with healthy aging in China can help policymakers and planners address the looming shortage of caregivers and improve the health and well-being of older adults.
References
1 United Nations (UN), World Population Prospects 2019, https://population.un.org/wpp/DataQuery/.
2 Yi Zeng, “Towards Deeper Research and Better Policy for Healthy Aging—Using the Unique Data of Chinese Longitudinal Healthy Longevity Survey,” China Economic Journal, 5, no. 2-3 (2012): 131-49.
3 World Bank Open Data, https://data.worldbank.org/.
4 James P. Smith, John Strauss, and Yaohui Zhao, “Healthy Aging in China,” Journal of the Economics of Ageing 4, no. 2 (2014): 37-43.
5 Yi Zeng et al., “Improvements in Survival and Activities of Daily Living Despite Declines in Physical and Cognitive Functioning Among the Oldest-Old in China–Evidence From a Cohort Study,” Lancet 389, no. 10079 (2017): 1619-29.
6 Hao Luo et al., “Health Expectancies in Adults Aged 50 Years or Older in China,” Journal of Aging Health 28, no. 5 (2016): 758-74.
7 Zuyun Liu et al., “Are China’s Oldest-Old Living Longer With Less Disability? A Longitudinal Modeling Analysis of Birth Cohorts Born 10Years Apart,” BMC Medicine 17, no. 23 (2019).
8 Overweight is classified as having a body mass index of 25 or more.
9 Smith, Strauss, and Zhao, “Healthy Aging in China.”
10 Smith, Strauss, and Zhao, “Healthy Aging in China.”
11 Xiaoyan Lei et al., “Living Arrangements of the Elderly in China: Evidence From the CHARLS National Baseline,” China Economic Journal 8, no. 3 (2015): 191-214.
12 Smith, Strauss, and Zhao, “Healthy Aging in China.”
13 Yi Zeng, “Options of Fertility Policy Transition in China,” Population and Development Review 33, no. 2 (2007): 215-46.
14 Toshiko Kaneda, Charlotte Greenbaum, and Kaitlyn Patierno, 2019 World Population Data Sheet (Washington, DC: Population Reference Bureau, 2019).
15 UN, 2018 Revision of World Urbanization Prospects, https://population.un.org/wup/ (2018).
16 Smith, Strauss, and Zhao, “Healthy Aging in China.”
17 Zhanlian Feng et al., “China’s Rapidly Aging Population Creates Policy Challenges in Shaping a Viable Long-Term Care System,” Health Affairs 31, no. 12 (2012): 2764–73.
18 Yi Zeng et al., “Implications of Changes in Households and Living Arrangements for Future Home-Based Care Needs and Costs of Disabled Elders in China,” Journal of Aging Health 27, no. 3 (2015): 519-50.
19 Smith, Strauss, and Zhao, “Healthy Aging in China.”
20 Feng et al., “China’s Rapidly Aging Population Creates Policy Challenges in Shaping a Viable Long-Term Care System.”
21 Chuanchuan Zhang et al., “Health Insurance and Health Care Among the Mid-Aged and Older Chinese: Evidence From the National Baseline Survey of CHARLS,” Health Economics 26, no. 4 (2017): 431-49.
22 James P. Smith, Meng Tian, and Yaohui Zhao, “Community Effects on Elderly Health: Evidence From CHARLS National Baseline,” Journal of the Economics of Ageing 1-2 (2013): 50-9.
23 Smith, Tian, and Zhao, “Community Effects on Elderly Health: Evidence From CHARLS National Baseline.”
24 Yuan Zhang and Eileen Crimmins, “Urban-Rural Differentials in Age- Related Biological Risk Among Middle-Aged and Older Chinese,” International Journal of Public Health 64, no. 6 (2019): 831-39.
25 Yuanxi Xiang et al., “The Impact of Rural-Urban Community Settings on Cognitive Decline: Results From a Nationally Representative Sample of Seniors in China,” BMC Geriatrics 18, no. 1 (2018): 323.
26 John S. Ji et al., “Residential Greenness and Mortality in Oldest-Old Women and Men in China: A Longitudinal Cohort Study,” The Lancet Planetary Health 3, no. 1 (2019): e17-25.
27 Tiantian Li et al., “All-Cause Mortality Risk Associated With Long-Term Exposure to Ambient PM2·5 in China: A Cohort Study,” The Lancet Public Health 3, no. 10 (2018): e470-477.
28 Xiaoyan Lei et al., “Gender Differences in Cognition in China and Reasons for Change Over Time: Evidence From CHARLS,” Journal of the Economics of Ageing 1, no. 4 (2014): 46-55.
29 Lei et al., “Gender Differences in Cognition in China and Reasons for Change Over Time: Evidence From CHARLS.”
30 Xiaomin Li et al., “Female Fertility History and Mid-Late-Life Health: Findings From China,” Journal of Women and Aging 30, no. 1 (2018): 62-74.
31 Ke Shen and Yi Zeng, “Direct and Indirect Effects of Childhood Conditions on Survival and Health Among Male and Female Elderly in China,” Social Science & Medicine 119 (2014): 207-14.
32 Shen and Zeng, “Direct and Indirect Effects of Childhood Conditions on Survival and Health Among Male and Female Elderly in China.”

 ">
">


