Mark Mather
Associate Vice President, U.S. Programs


The Voice for Data
In 2024, population aging and low fertility caught the world’s attention. Long predicted by demographers, these trends worked their way into the popular discourse—grabbing headlines, sparking debates, and filling PRB’s inboxes with questions from media, researchers, and the public.
These issues are complex, consequential, and real—yet, too often, they are reduced to alarmist coverage that obscures more than it reveals. At PRB, we believe that rigorous data and thoughtful analysis are essential to moving beyond headlines toward understanding and progress. Our mission—to use population data to help solve pressing societal challenges—has never been more critical.
To that end, we’re leaning into the evidence and making sure the insights they provide are widely—and freely—available, tempering those alarmist headlines with evidence-based context. It’s what we do so well here at PRB, and we know our work is vital to helping stakeholders understand many of the world’s most-pressing challenges.
Does every generation in the United States still do better than the last? What’s the economic value of unpaid care work? Is there really a population crisis because of low fertility? How can we prepare to meet the needs of aging populations? These are just some of the questions we addressed in Fiscal Year 2024.
Staff dug into the data and analyzed the impacts and implications of demographic changes in the United States and abroad. They also partnered with peers at organizations from around the world—from UNFPA Asia in Bangkok, Thailand, to the CREG Center in Theis, Senegal—to share findings with a global audience.
It was a year of speaking up and cutting through the noise with evidence. Every time. Accurate data and research are essential to our understanding of population dynamics and to crafting effective solutions to issues affecting people’s health and well-being.
My heartfelt thanks to all of you who supported our work this past year by attending a webinar, reading a report, sharing a post, funding a program, or donating a dollar. You helped us speak up as a voice for data in FY2024.
Sincerely,

President and CEO
“A young woman in the U.S. today, between the ages of 25 and 34, is more likely to die than at any point since at least the 1960s,” reports Sara Srygley, research associate at PRB.
“We’ve seen that young women today are doing many of the things they’ve been promised would lead to a better life, and these are things that worked in the past,” Srygley says. “Yet our research shows that despite their best efforts, they still face very real challenges compared with previous generations in some of the most fundamental areas of life.”
PRB’s original analysis of young women’s well-being shows that Millennial women ages 25 to 34 are doing worse on critical health and safety measures than women of the same ages from the Generation X and the Baby Boom generations. Today’s young women are more likely to die from preventable causes, be murdered, or die by suicide. These risks are even more pronounced for pregnant women.
A society is only as healthy its people are. Today’s young women face an uncertain future, marked by the erosion of rights and protections, complicated economic reality, and mental health tolls from the political, ecological, and social climates.
“How we address these threats to Millennial women’s well-being will set the stage for how Gen Z fares as they reach their young adulthood,” Srygley says.
PRB’s “Losing More Ground” report drove dialogue with experts and the media on poor state of women’s well-being in the United States. The findings reached more than 3 million people across print and digital media platforms, including coverage by CNN, ABC News, Axios, and Forbes.
We also partnered with The Center for Law and Social Policy, Justice and Joy National Collaborative, and Young Invincibles for a public discussion of the implications and potential policy solutions that would drive better outcomes for young Americans.
“We need to go beyond meeting just basic needs and try to build a system of benefits that is designed for people to thrive and experience abundance,” says Cara Brumfield, then a director at The Center for Law and Social Policy.
You can read the full report or hear from experts about why our findings matter.
“Since the 1960s, world population has more than doubled, but the growth rate has been falling the entire time,” says PRB’s Jennifer D. Sciubba in her TED Talk. “We’re witnessing the most fundamental shift to take place in modern human history.”
Two out of every three people in the world live somewhere with below replacement-level fertility (2.1 children per woman). From Canada to France to Japan to Türkiye, people are choosing to have fewer—or no—babies. And while fewer babies are being born, more people are living longer. China’s population aged 65 and older is expected to increase 85% by 2050.
“A country like the United States with low fertility—a shrinking and aging population—has dramatic implications, affecting everything from the health care workforce to transportation infrastructure,” says Beth Jarosz, Senior Program Director at PRB.
“People are the foundation of a society,” adds Sciubba. “We’re the workers and the voters and the soldiers and the caregivers. So, how many of us there are and who we are, that matters. We’re on track for there to be more people over age 60 than under the age of 14 by the middle of this century.”
A large older adult population will likely face challenges with financial stability, health, and caregiving. If countries don’t adapt to meet this shift, their social and economic systems could become overloaded. Labor costs and inflation will increase, social security systems could go bankrupt, and older adults will face a greater risk of poverty. All of these factors will make it even more costly for people to have children. “The question many world leaders should now be asking is how to plan for the strain that an aging and shrinking society puts on the care economy and the workforce,” Sciubba says.
We brought together nearly 500 people from across the globe and experts from the Peace Research Institute Oslo and Institute for the Future to discuss strategies for building a more resilient world in the face of population aging. Together with the UNFPA Asia and the Pacific Regional Office, we also briefed the media on demographic changes in the region and how policies can help support thriving aging populations. And we dug into the latest research on healthy aging to create a report, with funding from the Coordinating Center for the Centers on the Demography and Economics of Aging and Alzheimer’s Disease and Alzheimer’s Related Dementias, to highlight the importance of social connections in healthy longevity.
Rebecca Shamash of the Institute for the Future talked about how today’s technological boom could lead to massive productivity gains: “And if that was something that we could harness to really set ourselves up for this future world,…how could we use this technology to get us there a little bit faster, and to help us create more comfortable lives in the future?”
Check out the PRB x TED event, get highlights from the media briefing, or read more about social connections and aging.
“Primary health care helps people live longer, healthier lives, but nearly 50% of people in the world today can’t access quality care,” says Toshiko Kaneda, Technical Director of Demographic Research at PRB. “This is a serious challenge, and it will become bigger as the older adult population grows.”
When people can access quality primary health care at every stage of their life, they’re healthier longer. A healthier population can have a huge impact on maternal mortality and the burden of chronic diseases such as hypertension and diabetes that are commonly seen at older ages. It also lessens the demand for caregiving.
Access to good primary health care is already difficult for people across the globe, particularly in low- and middle-income countries. Many governments don’t have sufficient resources to meet their populations’ basic health needs, and skilled health professionals are overworked due to staff shortages, impacting the quality of care.
“The current struggle to access quality health care, combined with the projected near doubling of the global share of the population ages 65 and older by 2050, means health system strains will intensify. If investments aren’t made to improve access to good primary health care, the situation will be much worse 25 years from now, and the demand for caregiving, both paid and unpaid, will skyrocket,” says Kaneda.
We shined a spotlight on primary health care in the 2024 World Population Data Sheet, produced under the USAID-funded PROPEL Health project. This year’s Data Sheet featured 10 special indicators that reveal health spending per capita, use of family planning methods, health care workers per 10,000 population, and the Universal Health Care service coverage index for more than 200 countries and territories. We also created a media brief that journalists can use as a primer when reporting on the topic.
In 2024, over 1.3 million people accessed the World Population Data Sheet online, and 45,000 people downloaded the poster to use in classrooms and workplaces. Users got an inside look at the strength of primary health care in their countries—and how it compares to the rest of the world.
“Health spending from all sources per capita (US$) is $1,260 for the world and $74 in India, the most populous nation in the world. How might low investment in health care across populous nations affect global priorities and change the ability of governments and multilateral organizations to respond to events such as pandemics, migration, and climate change?” we prompt in the media brief.
Explore the 2024 World Population Data Sheet or learn how to report on this topic.
“Every adult has engaged in some form of care work,” says Cathryn Streifel, Senior Program Director at PRB. “But because of the differing expectations of roles for men and women, which inform how our societies are structured, most of it is done by women and is unpaid. Globally, women perform 76% of unpaid care work.”
Care work—the tasks involved in supporting others’ needs related to age, disability, or illness—is essential for human well-being, for societies to function, and for sustainable economic growth. Unpaid care work results from a lack of public investment in care services and infrastructure, and it comes with many costs, including substantial economic loss for uncompensated labor. Around the world, women regularly forfeit education and work opportunities to do the essential work of caring for children, older adults, and other family and kin.
“Women in Francophone West and Central Africa do the majority of domestic work, also called family care, and it keeps them out of school and the formal workforce. Because this work is unpaid, it remains invisible in Gross Domestic Product and in analyses of economic progress,” says Aïssata Fall, Africa Director at PRB. “In Togo, unpaid domestic work represents an estimated US$2 billion in social capital. And 30% of this work is done by women.”
“The United States also faces a serious burden of unpaid care work,” adds Beth Jarosz, Senior Program Director at PRB. “And it can have significant negative economic consequences, especially when that work is unpaid or underpaid. Combined with complex social safety net programs, the caregiving burden can limit women’s career opportunities, reduce their earnings potential, and increase financial hardship for women and their families.”
We collaborated with the CREG Center in Theis, Senegal, to develop a guidebook to support evidence-based discussions about unpaid care work with policy audiences in Francophone West and Central Africa. The real-world examples developed with local context provide a vital resource specifically for Francophone audiences. In the United States, we teamed up with Jessica Calarco, sociologist and author of Holding It Together: How Women Became America’s Safety Net, to discuss the issue in the United States with an expert panel including prominent advocates and researchers.
“[Y]ou can’t actually DIY society,” says Calarco. “Essentially forcing people to manage all that risk on their own has left many American families and communities teetering on the edge of collapse. And yet, … we haven’t collapsed in part because we have disproportionately women been the ones who are holding it together, filling in the gaps in our economy and the gaps in our threadbare social safety net.”
“It is not enough to simply recognize unpaid care work. It is crucial to understand its nature, scale, and age- and gender-related dynamics,” says Fall. “Without this understanding, there are risks of misdirecting public policy—or even reinforcing inequalities. Unpaid care work represents a major source of national wealth and well-being, yet it remains largely underestimated in current analytical frameworks.”
Explore the resource guide on unpaid care work, watch the webinar on America’s safety net, or visit the blog for webinar highlights.
“Postpartum hemorrhage is the leading cause of maternal mortality across the world, which is astonishing because it’s largely preventable,” says Megan Ivankovich, head of the USAID-funded MOMENTUM Knowledge Accelerator project at PRB. “More than 90% of these deaths occur to women in low- and middle-income countries.”
Postpartum hemorrhage occurs when the mother experiences blood loss of 500 milliliters or more within 24 hours after birth, according to the international definition. That’s more than 16 ounces, or over half a liter. Each year, about 14 million women around the world suffer from postpartum hemorrhage—and 70,000 die.
“Despite postpartum hemorrhage needlessly stealing mothers away from their families, there’s no consistent data collection on the condition. In fact, there’s a lot of disagreement about the factors involved, from the amount of blood loss to clinical signs and symptoms,” says Ivankovich. “We’re missing critical evidence that could save lives.”
The Sustainable Development Goals aim to reduce maternal mortality to 70 deaths per 100,000 live births by 2030, but 2023’s rate of 197 deaths starkly demonstrates that the world has a long way to go to reach this target. Around 70% of maternal deaths occurred in sub-Saharan Africa, and about 17% occurred in southern Asia, reports the World Health Organization.
We organized a webinar and two studies under USAID MOMENTUM to share guidance and tools with officials in health care and government and other health practitioners on the use of medications that aid uterine contractions and reduce postpartum hemorrhage but can also harm mother and baby. PRB project staff shared research, tools, and learning with 233 participants from 64 low- and middle-income countries on how to safely use these medications, called uterotonics.
“The webinar [was] a practical session with evidence relevant to the settings in which I am operating, and the operational research can be adapted,” says one participant from Kenya Amref Health Africa. Another participant from Cambodia shares that they “could use [the information] as an up-to-date resource to support the Midwifery Curriculum update in Cambodia.”
Our activities helped inform the uterotonics agenda for India’s Ministry of Health and Family Welfare and the Federation of Obstetric and Gynecologic Societies of India, who are developing enhanced guidelines on uterotonic use.
Learn more about uterotonics.
“There are too few young Americans and future workers being born to replace retirees,” says Diana Elliott, PRB’s Senior Vice President of Programs.
The United States had 1.4 million fewer workers than jobs in 2024. The absence of so many people from the workforce significantly impacts tax structures, distribution of tax burden, ability to repay debt, and GDP, as well as population dynamics.
The United States is confronting a demographic future of fewer workers while its population ages 65 and older grows rapidly. At the same time, changes in mortality and illness may be contributing to long-term labor force challenges. Policymakers can intervene to better engage workers who have been sidelined, such as people with disabilities and families with young children; support a wider variety of educational paths for employment; and evaluate wages and regulations.
“In the news, you may hear complaints about how young people aren’t working,” Elliott says. “In fact, there just aren’t as many young people to fill roles, which makes workforce training programs all the more important in the larger U.S. context.”
We got together with the Critical Labor Coalition and former U.S. Secretary of Labor Alexander Acosta for an open exchange about what the latest workforce data mean and how they could be used to develop short- and long-term responses to meet the challenge—individuals from over 40 countries joined in to ask questions and share ideas. And we spoke with media like The New York Times about the demographic factors involved in the U.S. labor shortage.
“Do we really treat all tracks equally and say, is the goal a family-sustaining wage, or have we started biasing the conversation in favor of those that have our backgrounds?” asks Secretary Acosta. “All of us on this talk on this panel went to college … if you look at the labor force data, you see that the biggest declines are not among the college graduates, but among those that didn’t go to college. And what are we doing to address them?”
“Accurate population data are critical for understanding our communities and planning for the future. So when decisionmakers can’t get the data they need, plans can miss the mark—with serious consequences,” says Mark Mather, Associate Vice President of U.S. Programs at PRB.
The U.S. Census Bureau collects and publishes vast amounts of data on the country’s population characteristics through the decennial census and the American Community Survey, but these raw data can be difficult to use. The Census Bureau also isn’t always informed on what data users need to know about the data to meet their communities’ needs.
“If decisionmakers and planners can’t track social and economic change where they live—things like workforce development, health insurance coverage, and child poverty and well-being—they can’t support people as their needs change,” says Mather. “A strong data infrastructure is critical to sustaining a healthy society.”
Comprehensive population data can help data users and others in government, business, academia, and nonprofits better understand and support their communities.
We teamed up with the U.S. Census Bureau and the Southern California Association of Governments to share resources, tools, and shortcuts with hundreds of data users across the United States. We met people in their communities, working with the University of Utah, Texas Demographic Center, the New York Law School, and the New York City Department of City Planning to host “ACS on the Road” events in Salt Lake City, Austin, and New York . With these tools at hand, they can more easily access and use U.S. population data in the American Community Survey (ACS) and better serve their communities’ needs.
“Are you finding that the data you need are not published in these estimates? … What do the data look like on a daily basis? And finally, with the tool or tools you are using, what limitations do you face accessing ACS data?” asks Mary Ana McKay, survey statistician in the American Community Survey Office. “These questions might have different answers depending on the day or the data you need.”
Which tool to use, she says, is “all about the best way to address your needs.”
Get tips on ACS data resources and discover data users’ needs.
“If countries are to make the most of their annual budgets, they need to have a clear understanding of how their investments performed in the past and of current and expected population needs. So, data collection, data analysis, and transparency of the budgeting process are key factors in developing effective public budgets,” says Reena Atuma, Activity Manager for this work at PRB.
Where these elements are lacking, the health of societies may suffer as some budgets fall short of demands, and services and infrastructure struggle to meet community needs. Researchers and decisionmakers may refer to analysis of past budget performance, tools for demographic dividend-sensitive budgeting, and census data to effectively support their communities.
“The labor, time and cost required to conduct a population census and analyze the data are significant,” says Jennifer D. Sciubba, President of PRB. “When countries can’t complete the process, their policies and programs may not be as effective as they could be.”
Accurate and transparent data help countries track needs and decide where to direct limited resources for the greatest impact. Prof. Latif Dramani, President and Coordinator at the CREG Center, notes in our joint webinar that this often means prioritizing strategic investments in human capital—education and health—over the operational costs of government institutions.
Without proper analysis, countries may make more investments in sustaining governing structures rather than in developing economic ones. “So these countries cannot stand up on their own feet until they can really fix this issue and balance out the structure,” Prof. Dramani says.
We collaborated with the Union for African Population Studies (UAPS) on a report that spotlights how researchers across Africa are using census data in development planning. We also worked closely with civil society organizations, local government officials, and others on subnational health financing challenges and solutions in Kenya. This financing work is part of a larger effort across the continent to boost the capacity of local civil society organizations to advocate for and ensure accountability in health financing.
Together with CREG, we brought experts, parliamentarians, and ministers together in West Africa to discuss tools that help countries harness the demographic dividend through budgeting. Our combined efforts opened high-level political dialogue between policymakers, ministry technical staff, and civil society on how age and sex shape people’s ability to fully participate in economic growth. This dialogue aligns with ongoing efforts to integrate unpaid care work into public policies.
“The [demographic dividend sensitive budgeting, BSDD] framework had influenced national strategies and opened dialogues between ministries, parliamentarians, and civil society,” says Astou Diouf, Director of Gender Equity in Senegal’s Ministry of Women, Family, Gender, and Child Protection. “These studies have enabled us to make recommendations to decisionmakers before the budgeting and point out priority for action.”
“[T]he results that have been shown by the scientific research show us that BSDD can really benefit us in taking advantage of the demographic dividend,” says Dr. Larba Issa Kobyagda, Director General of Economy and Planning, Ministry of Economy, Finance, and Development in Burkina Faso. “… [W]e must work so that the results of this research do not remain disconnected from policies, from politics.”
Explore how census data are used across Africa; hear more about budgeting processes for a demographic dividend; watch the webinar on strengthening budget systems in Africa; and read about domestic health financing in Kenya.
Webinar: Where Is the Workforce? Understanding the U.S. Labor Shortage and Working Toward Solutions
College Degrees Yield Lifetime Benefits for Disadvantaged Students
Five U.S. Facts and Trends in 2023 That You Should Know
Population Bulletin: Census Across Africa: Using Census Data for Policy and Planning
Should We Despair Over the Demographic Divide?
3 Bright Spots for Rural Appalachia—and 3 Struggles Compared to the Rest of Rural America
How Can Korea Respond to Its Population Crisis?
PRB Africa Highlights the Importance of Youth in Sustainable Development Work
PRB and CREG Share Tools for Capturing the Demographic Dividend in Senegal
PRB and Population Association of America Brief Congress on Maternal Death Crisis
A Patchwork of Access: Self-Managed Medication Abortion in Post-Roe America
PRB Kenya Presents at Nairobi Health Financing Conference
Race/Ethnicity Categories in Federal Surveys Are Changing: Implications for Data Users
Inaugural ACS on the Road Event Connects Texas Data Users With Census Bureau Staff
American Community Survey Resources, Shortcuts, and Tools Workshop
RTAC Partners Share End-of-Project Accomplishments and Impacts
The False Narrative of an Africa Unscathed by COVID-19
Citizenship, Ancestry May Help Determine Who Gets the ‘Hispanic Health Advantage’
College Shapes Black, White, and Latina Women’s Work and Family Lives Differently
Crowded Coasts Put 1 in 10 Americans at Risk for Floods, Other Hazards
Webinar: Writing About Population Research for Non-Scientists
From Paper to Practice: How PRB Supports Researchers to Put Their Results Into Action
Rural America Is Aging—Without Enough Care Workers
Webinar: How Women Became America’s Safety Net
Why Better Care Policies Matter for Gender Equality and the Economy
In Togo, PRB and CREG Discuss Importance of Recognizing Unpaid Care Work With Women Leaders
Fact Sheet: Aging in the United States
More Than Shelter: How Housing Affordability Is Linked to Older Americans’ Health
New Biomarker Research Provides Insights Into What Speeds up or Slows Down the Aging Process
No Matter Where They Lived, Older Americans With Dementia Were More Likely to Die From COVID-19
10 Things to Know About Older Americans’ Mental Health During the Pandemic
Safer but Alone: How COVID-19 Protections Affected Older Adults’ Mental Health
A Shift in Hunger: U.S. Food Policy and What We Learned From the Pandemic
In the Nest: Did the Pandemic Push More Young Adults to Live With Their Parents?
Is Your Child Misbehaving? Try Reasoning With Them
The Rise of the No-Bachelor’s Bachelor?
Expanded SNAP Benefits Boosted Food Security During the COVID-19 Emergency, Study Finds
![]()
The generous support we receive from organizations and individuals helps make our work possible. Thank you.
PRB worked alongside 15 organizations in 2024.
Through their generous contributions, the individuals listed here made it possible for PRB to fund essential program expansion and organizational innovations during the fiscal year ending Sept. 30, 2024.





Exploring New Ways to Use Data for Good
Since Population Reference Bureau’s (PRB’s) founding in 1929, the world has changed tremendously and PRB has evolved along with it. We continue to explore new ways of working (globally, locally, even remotely) and hone our expertise to offer solutions relevant to today’s health and well-being challenges, such as the growing prevalence of noncommunicable diseases and the increase in anxiety among young people. What hasn’t changed is PRB’s impact on informing evidence-based practices, which you’ll see highlighted in this report.
In Fiscal Year 2023, we reached wide audiences with analyses and assessments on issues such as population aging, climate adaptation, maternal health, unpaid care work, and big data. We partnered with organizations like the Conrad N. Hilton Foundation, Regional Consortium for Research on Generational Economy, Southern California Association of Governments, and William and Flora Hewlett Foundation. And the people who work here have made it all possible.
Part of any organization’s evolution is change in those people. From PRB’s original staff of 8 to 55 today, we’ve seen a lot of great people walk through our doors. In late 2022, we welcomed a new Vice President to lead our U.S. Programs, Diana Elliott. Midway through 2023, we appointed our first Africa Director, Aïssata Fall. And just a few months ago, PRB’s Board of Trustees appointed me as President and CEO. PRB’s new leadership is guided by the organization’s strategic plan to explore new areas of focus and ways of working while keeping population and demographic data at the core of what we do. It is a strong foundation from which to move forward toward our 100th year in 2029.
Our partners outside the organization are also essential to PRB’s success. My predecessor, Jeffrey Jordan, collaborated with other international organizations in 2023 on the TIME Initiative, an ongoing effort to answer hard questions about the evolving role of international nongovernmental organizations working in sexual and reproductive health and rights. I am pleased to be stepping into this space as I take the helm at PRB.
Barbara Seligman, Senior Vice President of International Programs, led the way in making PRB’s presence more prominent in 2023 as she advocated for our return to hosting more public events like the webinar on young Africa’s potential to power the global workforce. Diana Elliott quickly became another energetic force behind PRB’s increased public engagement, from authoring blogs that delve into the heart of current population concerns to speaking with the media and other organizations. And Reena Atuma, our Team Lead in Kenya, works daily alongside staff and local officials, youth, and others on concrete policy changes aimed at improving people’s health.
There’s so much more. We’ve captured some of the highlights for you in this year’s annual report.
Sincerely,

President and CEO

![]()
Under the PROPEL Health project, we worked with partner radio stations and community youth in nine districts across Malawi to raise awareness of social challenges around topics concerning nutrition, education, and health services; and harmful cultural norms like child marriage. We supported these local actors in their efforts to make context-specific, change-oriented information on these topics available in their communities and get people talking about them.
And they’ve made an impact.
Local radio programs in Malawi are now using their platform to hold leaders accountable for enforcing the child marriage law, and they are educating communities on how to respond to and prevent gender-based violence.
After a series of radio programs on child, early, and forced marriage and gender-based violence aired, a traditional authority in Monkey Bay in Malawi’s Southern Region publicly committed to enforcing the law against child and forced marriage, stating, “Dzimwe Radio has been insisting that I intervene and show my commitment in dealing with child marriages—hence my order to demote those village heads [found to not be enforcing the law].” In Mchinji, in Malawi’s Central Region, local police began holding town meetings about gender-based violence, and community members involved police and victim support units in investigations that led to the dissolution of child marriages, and arrests and fines for adult perpetrators.
And after Mudzi Wathu Radio aired programs about youth mental health challenges and the lack of available care, Mr. Biziwiki Mwatibu Banda, the clinical officer at Mchinji District Referral Hospital, announced, “We are very thankful to Mudzi Wathu Community Radio for giving youth a platform to express their views and present their complaints… After hearing those complaints, our management decided to train one health care provider from each of the 21 health centers, aiming to provide mental health counseling in all rural areas.”

In the process of spurring these positive changes—and many more like them—the young people involved in this work learned valuable skills that help provide them with more academic and professional opportunities.
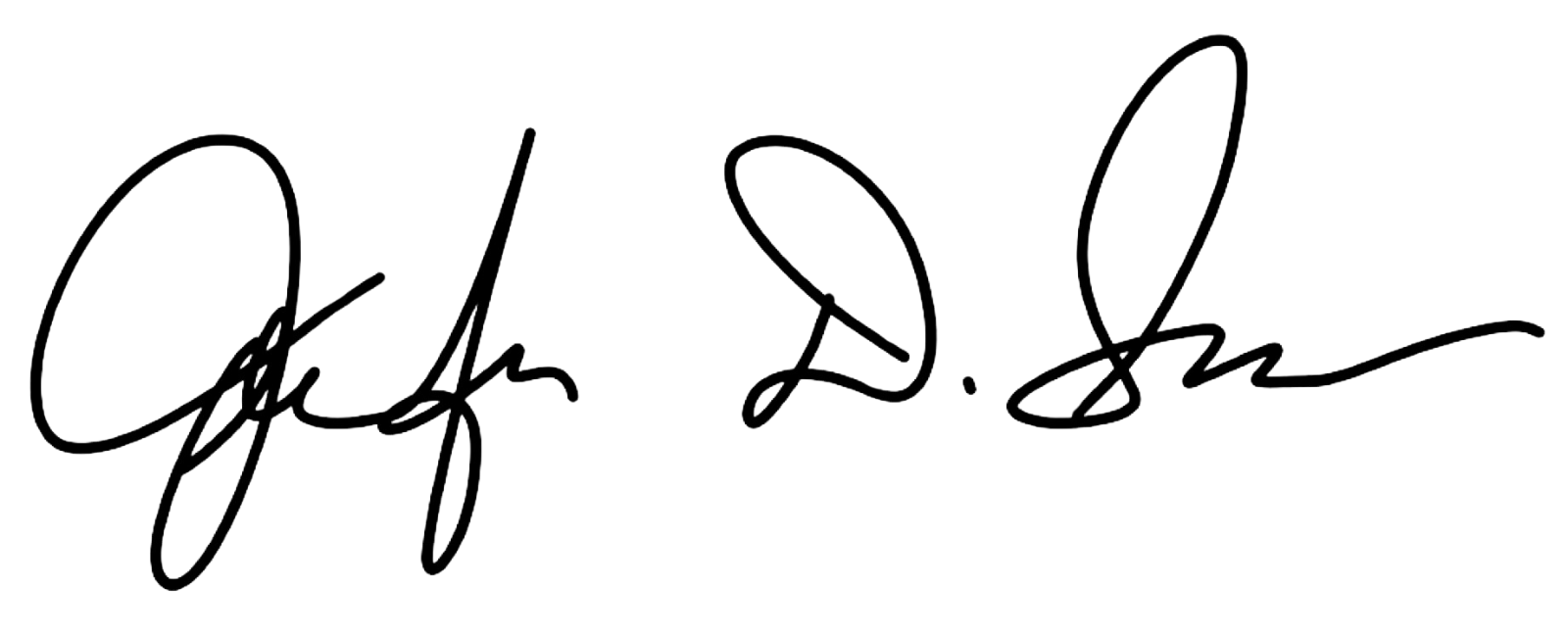
Black women in the United States face a high risk of death from pregnancy-related complications. Most of these deaths are preventable, according to a study by the Centers for Disease Control and Prevention. “We need new models of care before, during, and after birth to address these inequities,” says Marie Thoma, a reproductive and perinatal epidemiologist and population health scientist at the University of Maryland.
To raise awareness of the Black maternal health crisis in the United States, PRB partnered with creative agency TANK Worldwide and Dr. Shalon’s Maternal Action Project on a 2023 national campaign. It featured data from PRB’s article on NICHD-funded research that found U.S. Black women are 3.5 times more likely to die of pregnancy and postpartum complications than white women. With our partners, we promoted the campaign and research through social media, a press release, and fact sheet, and caught the attention of media, including NPR’s Here and Now. The campaign won a Clio Health award, which recognizes creative marketing and communications in the fields of physical, mental, and social well-being.
Read our follow-up interview with Marie Thoma about emerging research on this crisis.
How can local learning drive global solutions? This question is one we ask daily on the MOMENTUM Knowledge Accelerator project, which is part of USAID’s larger MOMENTUM program that seeks to improve the health and well-being of women, children, and families in more than 38 countries. Part of the project’s role is to identify and share best practices that can be applied across the different settings where MOMENTUM works.
In 2023, MOMENTUM Knowledge Accelerator brought together project staff who are working with their country counterparts to adopt and adapt the World Health Organization’s model of care for small and/or sick newborns in Indonesia, Mali, Nepal, and Nigeria. The goal? Develop a set of common questions and tools to learn about the model’s early rollout in different settings. For instance, how acceptable is the model in these settings? How feasible is it to implement the model in the different country contexts and settings? What adaptations are needed to the model based on the health systems’ contexts? The experiences in each country so far show that when health system and community actors are properly engaged, the model is acceptable, appropriate, and feasible in each setting. If governments can continue to provide resources to support the model’s different elements, more newborns can survive and thrive.
Using this information, we are working to share common approaches and address factors like how different aspects of the health system and variations between the public and private sectors affect the model’s implementation. Identifying and sharing such early insights can help shape global learning and strengthen the quality of care that small and sick newborns receive from their local health care providers—changing and improving lives.
This example is just one of the ways that we collaborate and communicate, gathering and assessing knowledge to share insights that people can put into practice.

Resources—and financial burdens—flow from one generation to another. Understanding how it happens is key for governments focused on fostering sustainable development, and data from national transfer accounts (NTA) can provide key insights.
In 2023, PRB and the Regional Consortium for Research on Generational Economy (CREG) hosted a shared space in Senegal to make complicated topics like the value of women’s unpaid labor easy to understand so decisionmakers could assess needs and accountability. The 3rd National Transfer Account–Africa Conference in La Somone-Senegal, held in partnership with CREG, PRB, the United Nations Population Fund, and United Nations Economic Commission for Africa, brought together more than 130 participants from 19 African countries, including parliamentarians and decisionmakers from various ministries.

The Africa NTA Network, drawn by our reputation for facilitating high-level policy dialogue informed by data, chose PRB to moderate three of four plenary conference sessions. Africa Director Aïssata Fall facilitated a session on the importance of unpaid care work and achieving a demographic dividend, which featured key messages developed by PRB policy communication fellows participating in the conference. She also directed two plenary sessions focused on high-level policy dialogue with parliamentarians and decisionmakers from ministries of planning, budget, gender, and social affairs. They came together to discuss challenges related to the demographic dividend and the care economy and the difficulty of translating these complex and often-abstract concepts so they can be considered in practical applications.
We developed a three-part climate blog series in English and French to advance a new approach to investments in climate adaptation that integrate population, gender, health, and the environment. The series lays the foundation of a people-centered framework for building resilience to climate change centered on agency, equity, and the power of local solutions.
And, in a year that closed as the hottest on record, solutions are more urgent than ever, as is knowing how—and which—populations will be most affected by climate change. Population characteristics like age, gender, and socioeconomic status are a few of the factors that make some people more vulnerable to the effects of a changing climate. Understanding them can help countries adapt and build resilience to future climate-related events, and we put a spotlight on this topic in our 2023 World Population Data Sheet.
We also worked with researchers participating in the 2023 ARUA Climate Change and Inequalities Symposium at the University of Cape Town to provide feedback and coaching on their presentations, which were focused on social inequalities and climate change action, so they could deliver clear, compelling messages. Read our top five tips to make your presentation message stand out.
The year 2023 marked the official end of the COVID-19 state of emergency. Yet the disease continued to spread, and many people continued to feel its effects. Decisionmakers need evidence of these impacts so they can effectively plan for their communities.
PRB’s KidsData program released data and findings from the Family Experiences During the COVID-19 Pandemic survey that highlighted ongoing challenges. The survey checked in with parents and caregivers four times to track the pandemic’s evolving impact on families. The results released in 2023 showed persistent challenges for California families despite suggestions that life had returned to normal.

In California, three years after the pandemic’s onset, children still faced significant COVID-related challenges, and their caregivers remained concerned. As safety-net supports began to roll back, nearly half of parents and caregivers statewide (45%) said their household finances were negatively impacted since the start of the pandemic, up from 32% a year prior. And more than half (58%) said they worried for the safety of their children as public health measures, like masking mandates, relaxed. Rates of concern were even higher in households with children with special health care needs.
The pandemic’s effects on young people are of particular concern as adverse childhood experiences, especially in early childhood, can have negative, long-term impacts on health and well-being. KidsData remains committed to tracking and analyzing data on the health and well-being of California’s children.
How can gender-transformative approaches and programming help improve outcomes for family planning and reproductive health? How can we address the gender inequities that global health workers experience? What are the links between sexual and reproductive health and technology-facilitated gender-based violence? What intersectional approaches are being applied to gender-transformative programming? How can comprehensive sexuality education help strengthen gender-based violence prevention and response efforts and vice versa?
If you are among the more than 2,600 members of the Interagency Gender Working Group (IGWG), you may already know the answers to these questions.
For 13 years, PRB managed the IGWG, a community of practice founded nearly 30 years ago to promote gender-sensitive considerations as a critical factor in improving family planning and reproductive health outcomes and advancing sustainable development.
Under our management, the IGWG highlighted best practices, challenges, and opportunities for promoting gender equality through global health programming, showcased the work of gender experts and advocates around the world, and led discussions on cutting-edge topics on and approaches to gender-transformative health programming.

In late 2023, we transitioned management of the IGWG to the PROPEL Youth and Gender project. During its time with PRB, the IGWG served as a reputable resource for gender experts, advocates, and program implementers working in global health and other sectors. It centered and elevated the voices of gender experts, advocates, and researchers, with special attention to locally led efforts, and the community of practice made notable contributions to the field with products that captured a wealth of knowledge and actionable recommendations for practitioners, advocates, researchers, and donors.
Both seasoned experts and those just beginning to integrate a gender-sensitive lens into their activities rely on materials like the IGWG’s newsletter and signature Gender Integration Continuum, a valuable tool for program implementers that measures whether and how interventions incorporate gender equity to improve development outcomes.
Explore some of our work with the IGWG:
We look forward to watching the IGWG’s continued growth and success.
As part of our activities on the Stawisha Pwani project, we collaborated with county officials, youth, and others in four coastal counties in Kenya as they sought to create and strengthen policies concerning the health of people in their communities.
We worked with officials in Mombasa County’s Department of Health to bring together youth representatives, county officials, and other stakeholders in the private sector and at nongovernmental organizations to develop the Mombasa County Adolescent and Young People Strategy on Health for 2024-2029. In our role of helping to facilitate dialogue, we drafted a template for the strategy and a plan for communicating its benefits to decisionmakers, and then formed a youth technical working group to draft, review, and revise the policy before it was shared with stakeholder groups for their feedback.

This collaborative process resulted in a strategy—approved by the Mombasa County government—that is in use today, helping to guide decisions across County departments on high impact programming for adolescents and young people.
In Taita Taveta County, we helped advance policy change by providing technical assistance to officials reviewing the Health Financing Facility Improvement Fund (FIF) law and developing the FIF operations and supervision manual. The FIF provides a way to collect and manage revenue from the health services delivered by public health facilities, as well as for these facilities to use the revenue to improve service delivery. The County and Subcounty Health Management Teams are relying on the manual as they monitor revenue collection to ensure resources are being used practically and to increase accountability.
The manual’s guidelines and revisions to the FIF law that allow facilities to retain and use revenue—a key element for strengthening health systems in Taita Taveta—contributed to the Department of Health surpassing its FIF collection targets for Fiscal Year 2022-2023. The Taita Taveta County Annual Development Plan 2024/25 reports that the collection goal of KES 100,000,000 was exceeded by more than 50%, for a total of KES 161,118,235. The health facilities can use these additional resources to further improve their efforts to meet the needs of the communities they serve.
![]()
PRB produced articles, blogs, reports, webinars, and other materials in 2023 on a range of topics such as climate adaptation, gender equality, population aging, unpaid care work, and the U.S. labor shortage. Explore some of these works here.
2023 World Population Data Sheet
A New Approach for Climate Resilience
Elements of Climate Resilience: The Foundations of a People-Centered Framework
Five Actions to Help Build Equitable Climate Resilience
Gender Equity for Work and Pay
Eight Demographic Trends We’re Watching as the World Population Passes 8 Billion
PRB CEO Calls for Restoring Public Trust in Data at United Nations Development Event
Comment l’autosoin peut soutenir la résilience en Afrique de l’Ouest et du Centre
How Self-Care Can Support Resilience in West and Central Africa
To Fix the Care Economy, the United States Should Look Internationally
Want Another Perspective on the U.S. Labor Shortage? Talk to a Demographer
The generous support we receive from organizations and individuals helps make our work possible. Thank you.
PRB worked together with 19 organizations in 2023.
Through their generous contributions, the individuals listed here allowed PRB to fund essential program expansion and organizational innovations during the fiscal year ending Sept. 30, 2023.

